Back to Annual Meeting Program
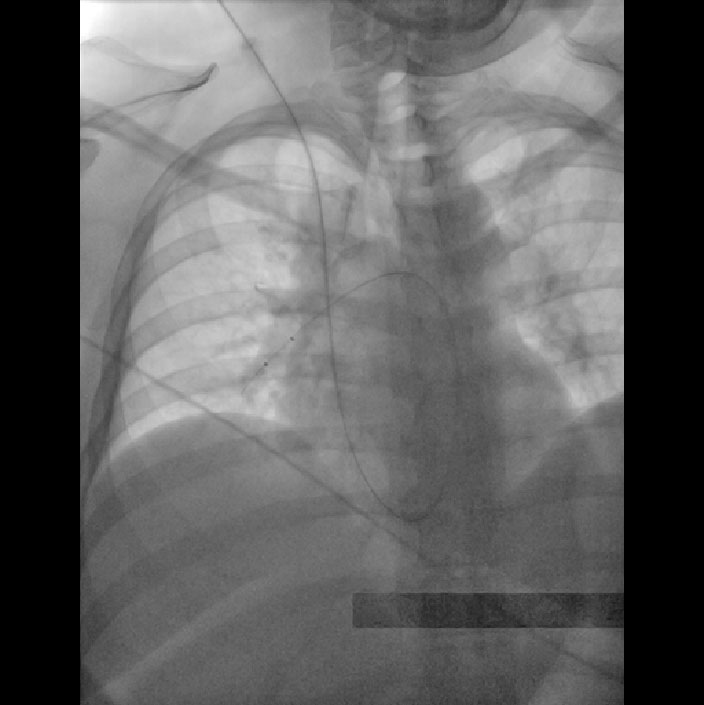
Catheter Directed Thrombolytic Therapy for Massive and Submassive Pulmonary Embolus: A Community Hospital Experience
Jeffrey Y Wang, Shan-ali Haider, Richard Silva, Michael Sulkin, Robert Fox
Shady Grove Adventist Hospital, Rockville, MD
INTRODUCTION: Pulmonary embolism (PE) is responsible for 200,000 deaths in the United States annually. Catheter directed thrombolytic therapy (CDTT) is reserved for massive and submassive PE, and rarely practiced outside of tertiary care university settings. Here we present a series of nine consecutive patients with massive (on pressors with hemodynamic instability) or submassive PE (echocardiograms showing pulmonary artery pressure > 70 mm Hg, right heart strain, and continued need for supplemental oxygen ) treated with CDTT in a community vascular surgery practice.
METHODS: Four patients were treated for massive PE and five were treated for submassive PE. All patients had been treated in intensive care units with systemic anticoagulation and significant supplemental oxygen requirement for as long as 5 days prior to being referred for lytic therapy. Upon referral, patients were treated with CDTT with powerpulse infusion of 10 to 15 mg of Alteplase into the left, right, and main pulmonary arteries. The decision to use mechanical thrombectomy was made at the time of procedure based on the patient’s clinical condition.
RESULTS: All nine patients were treated in a single setting. The mean age was 54.8±11.4 years, with 1 male and 8 females. The end point of treatment was weaning off pressors and/or decreased oxygen requirement. This was achieved in all nine patients (100% procedural success rate). One patient developed hemodynamically significant heart block with each attempt at powerpulse delivery, but was successfully treated with forceful injection through a running EKOS catheter. All patients were off supplemental oxygen within 24 hours of the procedure. There were no bleeding events in any patient. One patient expired 14 hours after the procedure with a suspected paradoxical embolus to the intestines (overall mortality 11%). The eight surviving patients were discharged to home within 48 hours of the intervention and had normal PA pressures without any evidence of right heart strain on echocardiogram performed one month after their CDTT procedure.
CONCLUSIONS: Massive or submassive PE can be treated safely with CDTT in a community hospital setting. This can reduce the need for lengthy ICU stays, shorten overall hospital length of stay, eliminate the need for home oxygen therapy, and restore right heart function with an acceptable mortality rate. Development of institutional CDTT expertise in conjunction with protocols to administer this therapy early in the course of massive and submassive PE may yield significant mortality and morbidity benefits in community hospitals.
Back to Annual Meeting Program
