Back to Annual Meeting Program
Treatment of Congenital Vascular Malformations Using a Multidisciplinary Approach: Results of a Prospective Study
Michael E Lidsky, Jovan N Markovic, Cynthia K Shortell
Duke University Medical Center, Durham, NC
Background: Vascular malformations (VM) are a rare and complex group of lesions which may present serious pitfalls in diagnosis and management. We sought to evaluate the safety and efficacy of our previously described imaging protocol and therapeutic algorithm in the treatment of low flow and high flow vascular malformations in a large series of patients.
Methods: A prospective database of all patients treated by the multidisciplinary vascular malformation team at our institution between 2006 and 2011 was reviewed. Management decisions were based on patients’ clinical profile as well as critical lesion characteristics, and included conservative care, sclerotherapy, embolization, surgical resection, or a combination of these modalities [Figure]. Treatment goals were established by the patient and physician at the time of initial evaluation. An outcomes grading system based on patient and physician derived treatment goals, and assessment of response to management was applied (1=worse; 2=unchanged, 3=significantly improved, 4=completely resolved), and post-procedural complications were identified.
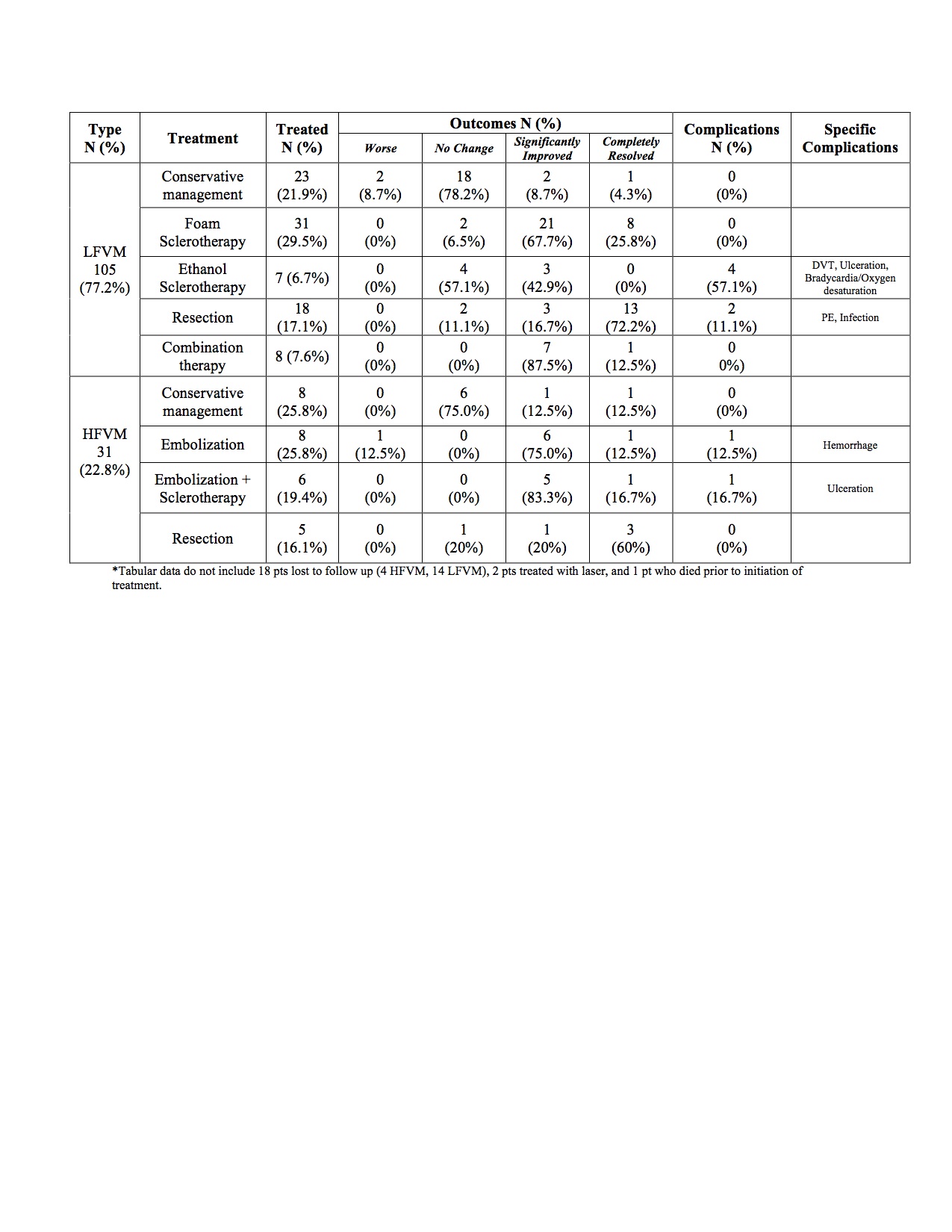
Results: The 136 vascular malformations in 135 patients included 59 (43.7%) males and 76 (56.3%) females, ranging in age from under 1 year to 68 years (mean = 25.3 ± 17.0). In order to facilitate application of the therapeutic algorithm, all patients underwent dceMRI to determine critical lesion characteristics including flow quality and lesion extension. Of the 105 (77.2%) low flow vascular malformations (LFVM), 23 (21.9%) were managed conservatively, 38 (36.2%) were treated with sclerotherapy (sodium tetradecyl sulfate, polidocanol, and/or ethanol), 18 (17.1%) were surgically resected, and 8 (7.6%) were managed with a combination of modalities. Of the 31 (22.8%) high flow vascular malformations (HFVM), 8 (25.8%) were managed conservatively, 8 (25.8%) were treated with transcatheter arterial embolization, 6 (19.4%) required embolization followed by sclerotherapy, and 5 (16.1%) were resected. Patients in all groups managed conservatively had minimal alteration in status. Response to sclerotherapy in the LFVM group resulted in improvement in 32 (84.2%) patients, surgical resection resulted in improvement in 16 (88.9%) patients, and combination therapy resulted in improvement in 8 (100%) patients. Treatment with embolization in the HFVM group resulted in improvement in 7 (87.5%) patients, while combination therapy resulted in improvement in 6 (100.0%), and surgical resection led to improvement in 4 (80%) [Table]. Complications were observed in 6 (6.8%) patients treated for LFVMs (0 with sodium tetradecyl sulfate or polidocanol, 4 with ethanol, 2 with resection), and 2 (7.4%) patients treated for HFVMs with embolization or combination therapy.
Conclusion: In this large cohort of vascular malformation patients, implementation of the proposed diagnostic and therapeutic algorithms in a multidisciplinary setting resulted in favorable outcomes with an acceptable complication rate in this challenging patient population. 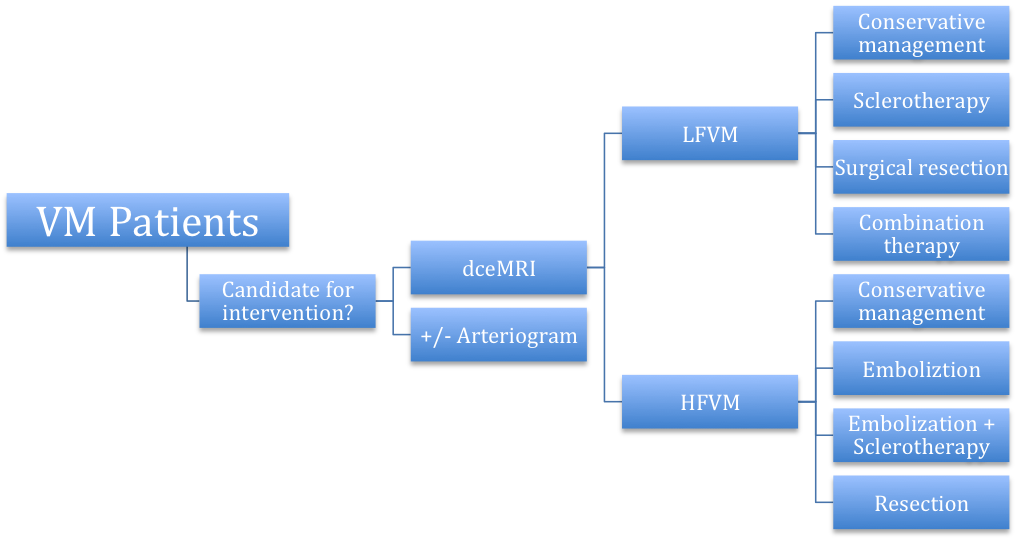
Back to Annual Meeting Program
