Back to Annual Meeting Program
Spliced Arm Vein Grafts For Critical Lower Limb Ischemia
Luigi Pascarella, Leila Mureebe, Mitchell W Cox, Richard L McCann
Duke University Medical Center, Durham, NC
INTRODUCTION: Many patients with critical limb ischemia do not have adequate ipsilateral saphenous vein for constructing a bypass due to prior harvesting for limb or coronary bypass or due to intrinsic vein disease. Prosthetic conduits or frozen or tanned homografts have poor long-term patency, especially for distal bypass. This study reviews our experience with an alternate conduit using spliced arm veins, for bypass of critical lower limb ischemia.
METHODS: A retrospective chart review was conducted of all patients at a single institution over a 11 year period. Statistical analysis was conducted by Kaplan Meier survival analysis and Cox proportional hazards model. Statistical significance was set at p=0.05.
RESULTS: Since 2001, 33 patients (22 male, 11 female, mean age 65), with critical limb ischemia underwent 34 bypass operations using a conduit containing at least one arm vein segment and one or more splices. All had rest pain or tissue loss and 70% had undergone prior bypass attempts (range 0-4, mean 1.3 prior bypasses). 20% of patients had undergone attempts at percutaneous revascularization. Conduits consisted of cephalic vein (N=16), basilic vein (N=32), and residual saphenous vein (N=24) segments. Six grafts (18%) had two splices. 85% of bypasses were to tibial vessels. Patency at one year was 100% (20/20) and at two years 85% (12/14, figure 1). One patient required amputation with a patent graft, and one patient underwent amputation after graft thrombosis. There was no statistical impact on amputation or patency based on source of vein, inflow artery, outflow artery, number of splices or patient age.
CONCLUSIONS: Spliced arm vein grafts provide durable lower extremity revascularization and limb salvage when intact saphenous vein is not available. Spliced arm grafts are superior to prosthetic or frozen homografts for repeat bypass after failure of an initial autogenous graft. 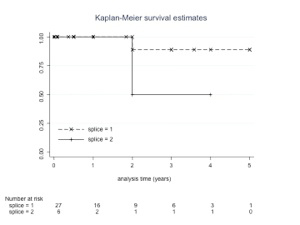
Back to Annual Meeting Program

