Back to Annual Meeting Program
A Novel Depletion Approach Attenuates A Surge Of CD34 Progenitors After Vascular Injury: Implications for Restenotic Vascular Disease
Bryan Tillman, Justine Kim, Adriana Harbuzariu
University of Pittsburgh School of Medicine, Pittsburgh, PA
Introduction: Intimal hyperplasia is an overactive healing response that leads to failure of half of all vascular interventions in under five years. Increasing evidence suggests that circulating progenitor cells expressing the marker CD34 play an important role in this disease. Several studies have highlighted either a direct cellular contribution to intimal lesions or by fostering a favorable environment for restenosis. Despite their evolving importance in this clinically important disease the kinetics of CD34 cell mobilization after vascular injury are not known. In addition, there is no way to specifically intervene on these cells. In this study, we investigated the timecourse of CD34 positive progenitor cells after vascular injury and examined whether an affinity pheresis approach could mediate systemic depletion of CD34 positive cells at the time of vascular injury in a large animal model.
Methods: An ovine model underwent placement of an arteriovenous PTFE graft between the carotid and jugular veins. The contralateral carotid underwent balloon angioplasty. Endothelial injury in this model was confirmed by scanning electron microscopy. The first groups of animals underwent flow cytometric assessment of CD34/VEGFR2 positive cells after vascular (n=3) and a control, non-vascular surgery (n=3). Next, separate groups of animals underwent vascular injury and over 14 days the model underwent serial depletion using affinity pheresis towards either the progenitor cell marker CD34 (n=3) or a mock control (n=4). Cells bound to the affinity system were eluted enzymatically and examined by flow cytometry. Finally complete blood counts were compared between our study groups for changes after affinity pheresis.
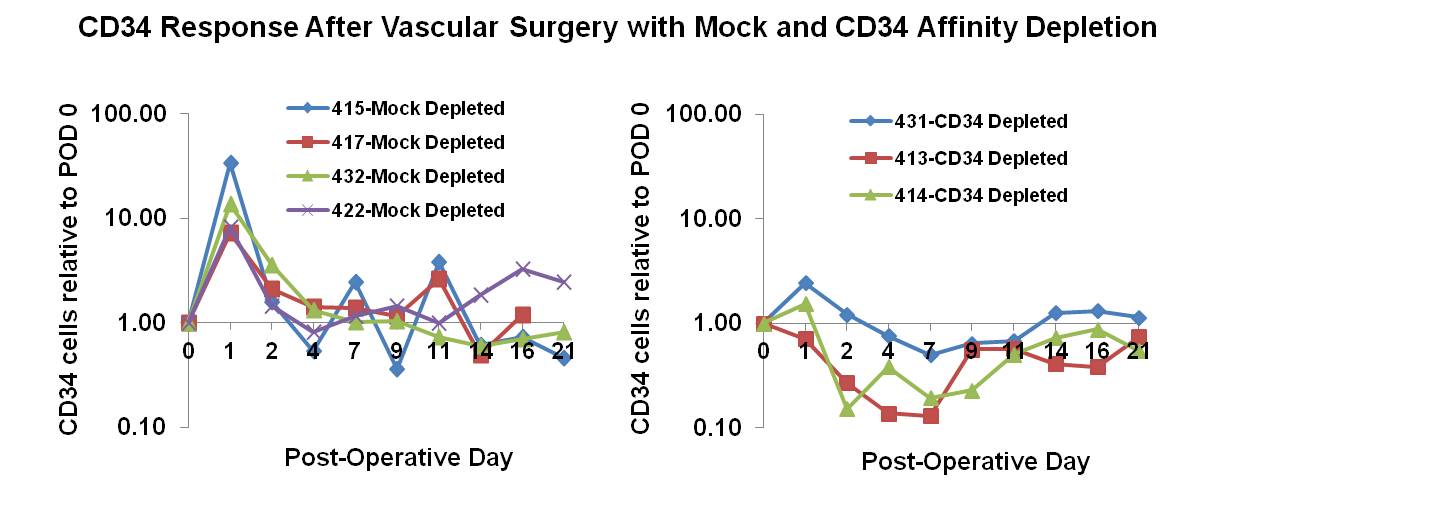
Results: Our findings suggest a surge of CD34 positive cells following vascular intervention that is not observed after control surgical procedures (Figure 1). Our pheresis group revealed that the surge can be attenuated by a CD34 affinity pheresis but not by a mock control (Figure 2). Consistent with these findings, cells recovered from the affinity cartridge reveal large numbers of CD34 positive cells that is not found in the control group. Finally, our findings revealed that even after multiple sessions of affinity pheresis device that complete blood counts remain essentially unchanged.
Conclusions: This study is the first to document a surge of CD34 positive progenitors that appears to be limited to macrovascular injury. This finding may have important implications on the pathology of vascular restenosis. We further conclude that CD34 affinity pheresis can mediate significant in vivo depletion of circulating progenitor cells. Our results also indicate that the specificity of this depletion has minimal impact on clinical measures of blood composition. Given the evolving role of these cells in the pathology of restenosis, this approach may have important clinical implications. Future studies will evaluate the implications of this depletion on recurrent vascular disease.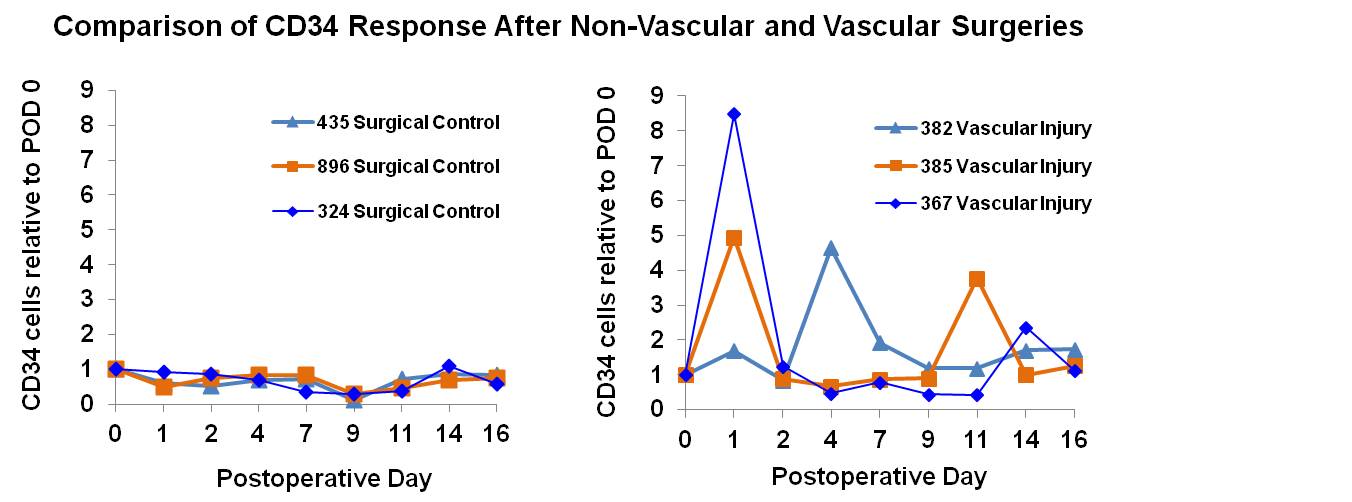
Back to Annual Meeting Program

