Back to Annual Meeting Program
Endovascular Repair of a Ruptured Subclavian Artery Aneurysm in a Patient with Ehlers-Danlos Syndrome Using a Sandwich Technique
Sapan S Desai, Maria Codreanu, Kristofer Charlton-Ouw, Hazim Safi, Ali Azizzadeh
University of Texas Houston Medical School and Memorial Hermann Hospital, Houston, TX
INTRODUCTION: A defect in collagen synthesis leads to extreme vascular fragility in patients with type IV Ehlers-Danlos syndrome. The majority of patients develop significant vascular complications by the age of 40. Open surgical repair remains a formidable challenge that is fraught with complications. We present the case of a patient with a ruptured subclavian artery aneurysm and associated arteriovenous fistula who underwent successful endovascular repair. Lack of a proximal seal zone in the subclavian artery aneurysm necessitated simultaneous stent graft repair of the innominate artery using a sandwich technique.
METHODS: A 17-year-old man with known type IV Ehlers-Danlos syndrome developed right neck and shoulder swelling following a sports-related cervical hyperextension injury. He was intubated on arrival for airway compromise. A CTA study demonstrated a 17 x 13 cm ruptured subclavian artery aneurysm with an associated internal jugular vein arteriovenous fistula. He was emergently taken to the hybrid operating suite for repair. An aortogram was obtained via an open right femoral exposure (Figure 1). The right brachial artery was exposed (8 Fr.). A wire was passed from the right femoral approach into the right brachial artery and retrieved through the sheath. A 7 mm x 15 cm stent graft (Viabahn, WL Gore & Associates, Flagstaff, AZ) was advanced from the right brachial approach into the innominate artery. Simultaneously, using a separate wire placed into the right carotid artery via the right femoral approach (7 Fr.), a 7 mm x 10 cm stent graft (Viabahn) was advanced into the innominate artery. The two stent grafts were aligned in the innominate artery using a sandwich technique to obtain a proximal seal zone. An additional 8 mm x 10 cm stent graft (Viabahn) was placed from the right brachial approach to obtain a distal landing zone in the axillary artery.
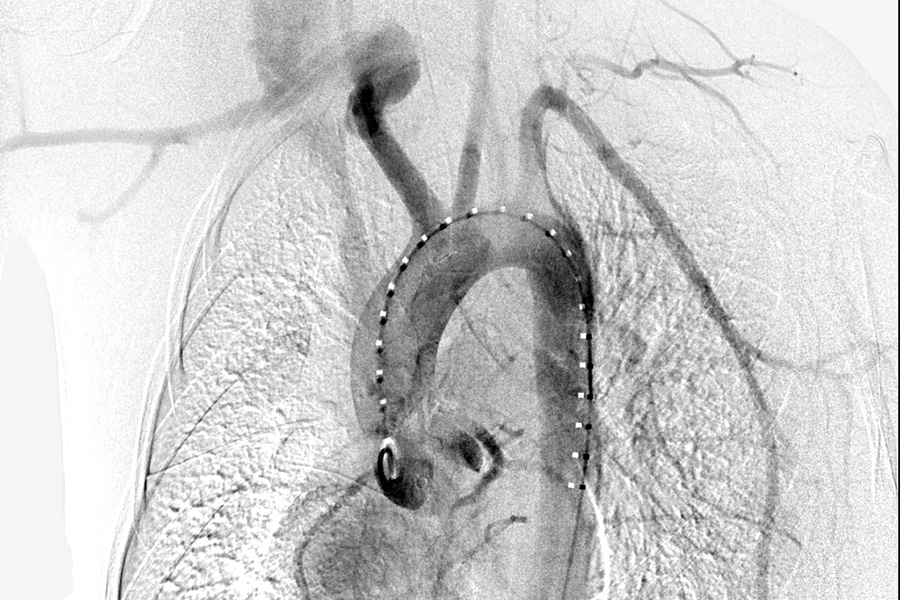
RESULTS: A completion angiogram revealed successful exclusion of the subclavian artery aneurysm and arteriovenous fistula (Figure 2). The brachial artery was repaired using a cephalic vein patch. The femoral artery was repaired primarily. The patient tolerated the procedure well with no complications. The neck swelling resolved. He was extubated on POD1. He had an uneventful hospital course and was discharged in stable condition on POD5.

CONCLUSION: This is a case a ruptured subclavian artery aneurysm in a patient with type IV Ehlers-Danlos syndrome who had a prohibitively high risk for open surgical repair. Lack of a proximal landing zone necessitated endovascular repair using a sandwich technique. The fragility of access vessels in this patient population may require patch repair. Use of this technique may be a suitable alternative to open repair in high risk patients.
Back to Annual Meeting Program

