Back to Annual Meeting Program
Endovascular Repair of Blunt Popliteal Artery Injury via Retrograde Tibial Access
Jeff Luh, Lori Choi, Charlie C Cheng, Z Faisal Cheema, Michael B Silva, Jr.
UTMB, Galveston, TX
Background. Popliteal artery injuries from posterior knee dislocations are associated with limb-threatening ischemia and amputation. Endovascular approaches to trauma surgery are gaining increased acceptance, especially for solid organ injury and aortic transections. We present a case of posterior knee dislocation with popliteal artery transection resulting in a pulseless extremity, in which revascularization was accomplished via a retrograde approach from percutaneous, ipsilateral posterior tibial artery access.Methods. A 34 year old man presented after fall from the bed of his truck. He complained of sharp pain to the posterior right knee and coldness of the calf and foot. Physical examination revealed an obese man (body mass index of 53) in mild distress. His Glasgow Coma Scale was normal and he was hemodynamically stable. His right popliteal region was ecchymotic, swollen and tender with decreased range of motion of the knee. The calf and foot were cold with preserved motor and sensory function. Popliteal, dorsalis pedis, and posterior tibial artery pulses were not palpable and Doppler signals could not be obtained. The patient was taken to the hybrid endovascular operating room within 1 hour of initial presentation for revascularization and placement of external fixator device. Via contralateral common femoral artery access, selective arteriography was performed the right superficial femoral artery (SFA). Thrombosis of the above knee popliteal artery, with reconstitution of the below-knee popliteal artery, was seen.
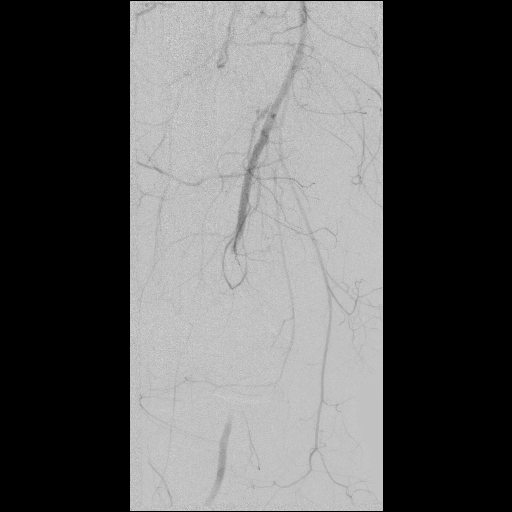
Attempts to cross the lesion from this antegrade approach resulted in perforation. Under ultrasound guidance, a 2.6 French sheath was placed in the posterior tibial artery at the level of the ankle. A wire was successfully passed from this access, through the occlusion and out the contralateral femoral artery access. A 6 millimeter diameter by 15 centimeter length covered stent graft was deployed across the lesion  . Completion arteriogram demonstrated restoration of prograde flow without extravasation or embolization.
. Completion arteriogram demonstrated restoration of prograde flow without extravasation or embolization.
Results: Distal pulses were palpable at the completion of the case. Motor and sensory function remained intact post-operatively and patient did not require fasciotomy. Plasma creatinine remained within normal limits. Estimated blood loss from these procedures was 80 milliliters. He was transferred out of the intensive care unit on post-operative day 1 and discharged on day 4 on clopidogrel. At 3 months’ follow-up, he remained in good condition with palpable distal pulses.
Conclusion. Endovascular intervention has the potential to lower blood loss, reduce surgical morbidity, and shorten procedure and recovery times from vascular trauma. Utilization of covered stents and filter wires with anterograde and retrograde access techniques can provide novel ways to manage popliteal artery injuries. Further investigation with long-term follow-up will be useful in determining the effectiveness and durability of these repairs.
Back to Annual Meeting Program

