Back to Annual Meeting Posters
Subclavian Revascularization in the Age of TEVAR: Comparison of Outcomes to Patients with Occlusive Disease
Salvatore T. Scali, Stephen G. Pape, Catherine K. Chang, Robert J, Feezor, Peter R. Nelson, Scott A. Berceli, Thomas S. Huber, Adam W. Beck
university of florida- gainesville, Gainesville, FL
INTRODUCTION:
Open surgical revascularization for subclavian artery occlusive disease(OD) has been supplanted by endovascular treatment despite the excellent long term patency of surgical bypass. The indications for carotid-subclavian bypass(C-S BPG) and subclavian transposition(ST) have been recently expanded with the widespread application of thoracic endovascular repair(TEVAR) to augment proximal landing zones or treat endovascular failures. This study was performed to compare the perioperative and long-term outcomes of patients undergoing C-S BPG/ST for TEVAR with those for OD.
METHODS:
A prospective database including all procedures performed at a single institution since July1, 2002 was retrospectively queried for patients who have undergone subclavian revascularization for either TEVAR or OD indications. Patient demographics and peri-operative outcomes were recorded. Patency was determined by computed tomographic angiography in the TEVAR group, while non-invasive studies were used for the OD patients. Life table methods were used to estimate patency, re-intervention and survival.
RESULTS:
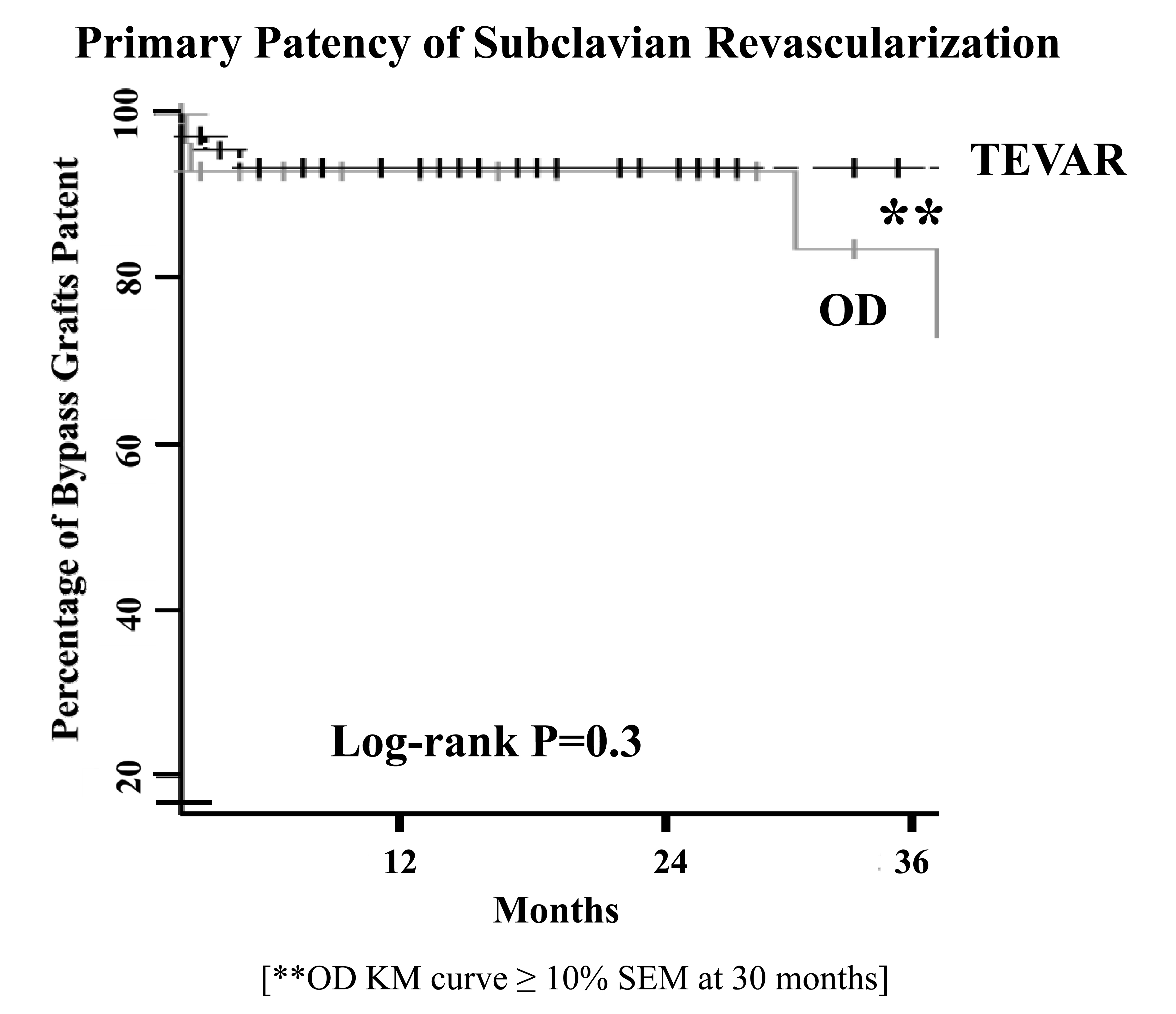
A total of 139 procedures were identified, with 101 performed for TEVAR, and 38 for OD. All TEVAR patients underwent C-S BPG/ST to augment landing zones (preoperative 49%; intraoperative 41%), treat arm ischemia (postoperative, 8%), or to salvage the internal mammary artery (2%). Patients with OD had a variety of indications [failed stent resulting in arm fatigue, 49%; asymptomatic, >80% cerebrovascular disease(CVOD) with concomitant carotid endarterectomy, 18%; symptomatic CVOD, 13%; redo bypass, 8%; and coronary-subclavian steal, 5%]. Significant differences in age (years±SD:TEVAR, 64±12 vs. OD, 59±12; P=0.05) and body mass index (TEVAR, 29±5 vs. 26±4; P=0.004) were present between the 2 groups. Despite the expected differences in prevalence of cardiovascular risk factors(Table), no differences in antiplatelet, anticoagulant or statin utilization were detected. There was no difference in the overall rate of postoperative complications(P=0.9). TEVAR procedures that required a C-S BPG/ST had a post-TEVAR stroke rate of 6.9% vs. OD, 10.5%(P=0.5). No significant difference was noted between the 2 groups in primary, primary assisted, and secondary patencies(Table, Figure).
CONCLUSIONS: In this contemporary series of C-S BPG/ST performed for TEVAR and OD indications, stroke risk may be higher than previously reported in historical series. In TEVAR patients, this may be attributed to the procedural complexity of the TEVAR in patients requiring subclavian revascularization. In OD patients, this is likely due to the changing patient population who require more frequent concomitant carotid interventions. Despite the short-term morbidity, excellent bypass durability and equivalent long-term patient survival can be anticipated. 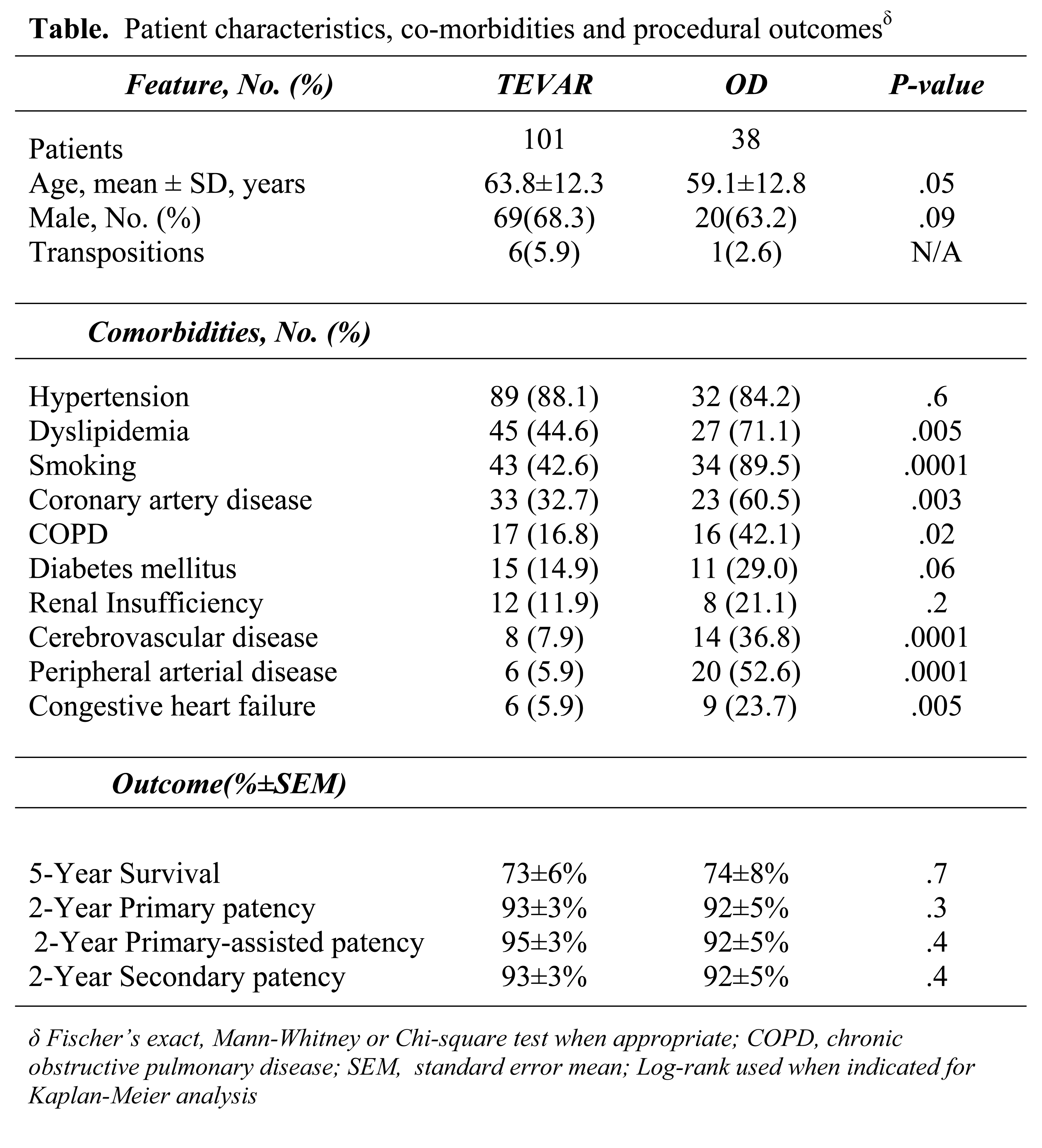
Back to Annual Meeting Posters

