Back to Annual Meeting Posters
Endovascular Treatment of Aortic Saddle Embolism Using Covered Stents, Effecting Full Neurologic Recovery
Jane K Yang, Alex Nguyen, Hilene de Amorim, Lee J. Goldstein, Arash Bornak
University of Miami, Miller School of Medicine, Miami, FL
Background
The majority of patients with aortic saddle embolisms will present with lower extremity motor and sensory deficit. These patients have traditionally been treated with surgical thrombectomy, either from the femoral arteries or from a direct aortic approach. We report the first case in the literature of an aortic saddle embolism treated endovascularly with covered stents. This technique preserved the pelvic circulation and allowed full neurologic recovery.
Methods
A 43-year-old female presented with a three-week history of worsening paraplegia and paresthesia.
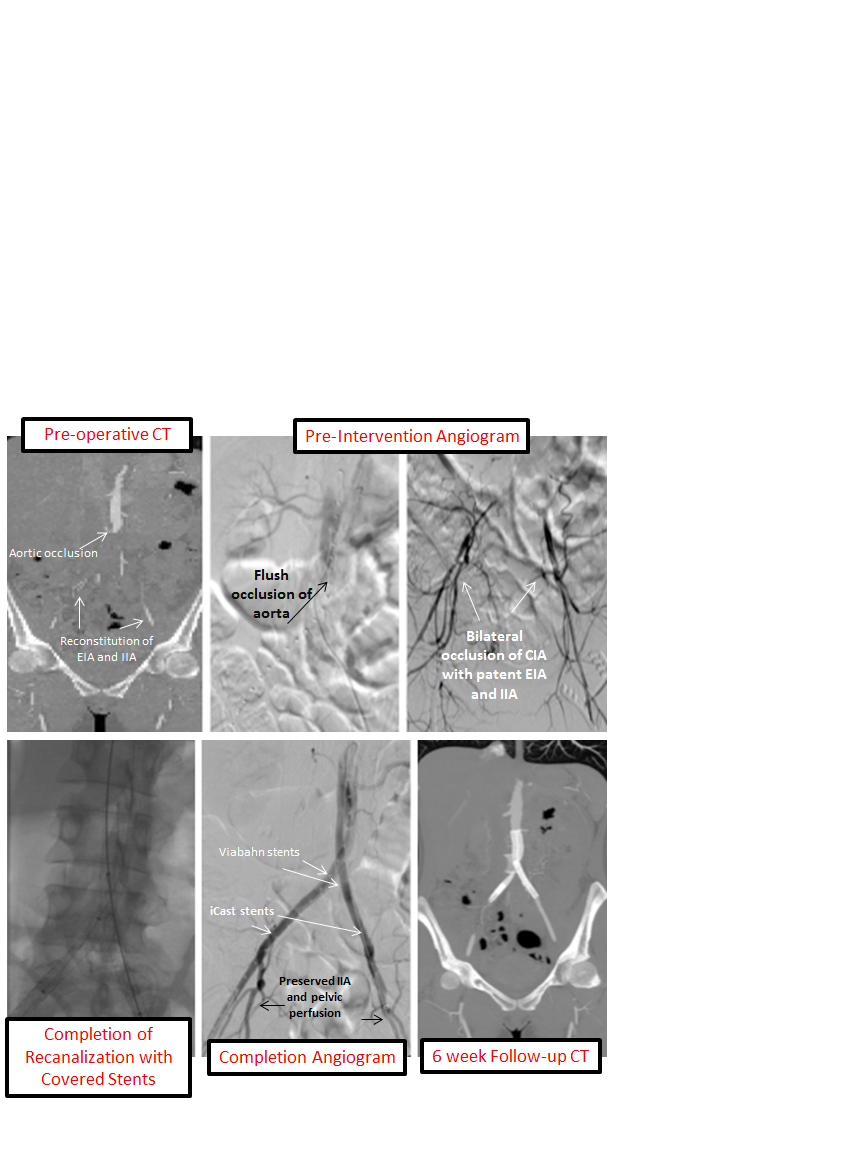
A CT angiogram demonstrated an aortic occlusion immediately distal to the origin of the inferior mesenteric artery and occlusion of the common iliac arteries (CIAs), but preserved flow in the internal (IIAs) and external iliac arteries (EIAs). Given the subacute nature of the symptoms, a spinal MRI was performed, which did not show any spinal infarcts.
The patient was taken to the operating room. Bilateral common femoral arteries (CFA) were controlled, distally clamped to avoid embolization, and directly accessed.
A Viabahn (Gore Medical, Flagstaff, AZ) self-expanding covered stent was advanced into each CIA, so that the top of each stent extended proximal to the aortic thrombus, and the two stents were deployed simultaneously. On each side, revascularization of the aorto-iliac segment and exclusion of the thrombus burden was completed by deploying an iCast (Atrium Medical Corp., Hudson, NH) balloon-expandable covered stent. Each iCast overlapped on one end with the Viabahn stent and at the other end apposed the distal CIA, preserving the internal iliac arteries and pelvic circulation.
Results
A completion angiogram demonstrated in-line flow from the aorta to both the EIAs and IIAs with complete exclusion of the saddle embolus. At the conclusion of this procedure, bilateral four-compartment fasciotomies were performed.
Post-operatively the patient had immediate neurological recovery with a residual left foot drop that resolved completely over the next six weeks with physical therapy.
Conclusions
Previous treatments for aortic saddle embolism involved surgical thrombectomy, which left a persistent residual thrombus burden in the aorto-iliac segment that could post-operatively embolize, and carried a significant risk of pelvic embolization.
The role and efficacy of covered stents in the treatment of chronic aorto-iliac occlusive disease has been reported in literature. Our case report is an example of covered stents used in a subacute setting. The treatment of an aortic saddle embolism was effectively performed with subsequent full neurologic recovery and no distal embolization. We believe that preservation of the pelvic perfusion through the IIAs was essential to maintaining spinal perfusion and protecting this patient from permanent neurological deficit. Our technique allowed complete and precise exclusion of the thrombus burden in the distal CIAs and prevented IIA embolization.
Back to Annual Meeting Posters

