Back to Annual Meeting Posters
Infected Endograft is a Dangerous Late Complication of EVAR
Gregory A. Stanley, Melissa L. Kirkwood, J. Gregory Modrall, Carlos H. Timaran, Jayer Chung, R. James Valentine
UT Southwestern, Dallas, TX
BACKGROUND: The long-term complications of endovascular aneurysm repair (EVAR) have been well documented and are primarily related to endoleaks and graft thrombosis. Modern case reports indicate that EVAR graft infections may become more prevalent, in part due to the increasing number of patients treated by EVAR and the routine use of postoperative surveillance imaging. However, experience with infected EVAR has been scant, and the outcome of treatment is unknown. The purpose of this study was to review our 5-year experience with infected EVAR at a referral center for prosthetic graft infections.
METHODS: We performed a retrospective review of consecutive patients diagnosed with EVAR infection at a tertiary care academic medical center from September 2007 to May 2012. Patient demographics, medical comorbidities, laboratory data, radiographic findings, operative details, and outcome data were collected from the electronic medical record.
RESULTS: During the five-year study period, eleven patients (all males, mean age 7110 years) were diagnosed with infected EVAR. Ten of 11 patients presented with clinical signs and symptoms of infection (fever, chills, malaise), while one was asymptomatic. The median time from initial EVAR placement to diagnosis of infection was 12 months (range, 4-84 months). Computed tomography was obtained in all patients to confirm the diagnosis, demonstrating air in the aneurysm sac in six patients and peri-aortic stranding in five others. After initiation of broad-spectrum intravenous antibiotics, all patients underwent rapid assessment of perioperative risk. Two patients were deemed unsuitable for operative intervention due to end-stage COPD and uncorrectable CHF; both were treated medically with lifelong antibiotics. The remaining nine patients underwent complete endograft explantation with revascularization using autogenous femoral vein (NAIS)(n=7), cryopreserved arterial homograft (n=1), or extraanatomic bypass (n=1). Seven of the nine patients were found to have duodenal erosion at the time of graft explantation, and duodenal repair was performed concurrently. Microorganisms isolated from blood cultures or surgical specimens included Staphylococcus species (n=5), Streptococcus species (n=2), Candida species (n=5), Enterococcus faecalis (n=4), Escherichia coli (n=2), and Clostridium septicum (n=1). Eight of 11 patients had polymicrobial infections. Surgically treated patients had a mean hospital length of stay of 18.57 days, and were discharged to home (n=6), to a rehabilitation center (n=2), or to a skilled nursing facility (n=1). There were no operative deaths, and all surgical patients were alive at a mean of follow-up of 25 months (range, 2-58 months).
CONCLUSIONS: Infected EVAR should be suspected in any patient with systemic signs of sepsis. The present data show that EVAR infection can present within months to as late as many years after original implantation, and associated duodenal erosion is common. Explantation of the infected endograft remains the mainstay of treatment in surgically appropriate patients. The optimal method of revascularization should be tailored to each patient, but reconstruction with autogenous femoral vein appears to be an excellent option for medically fit patients.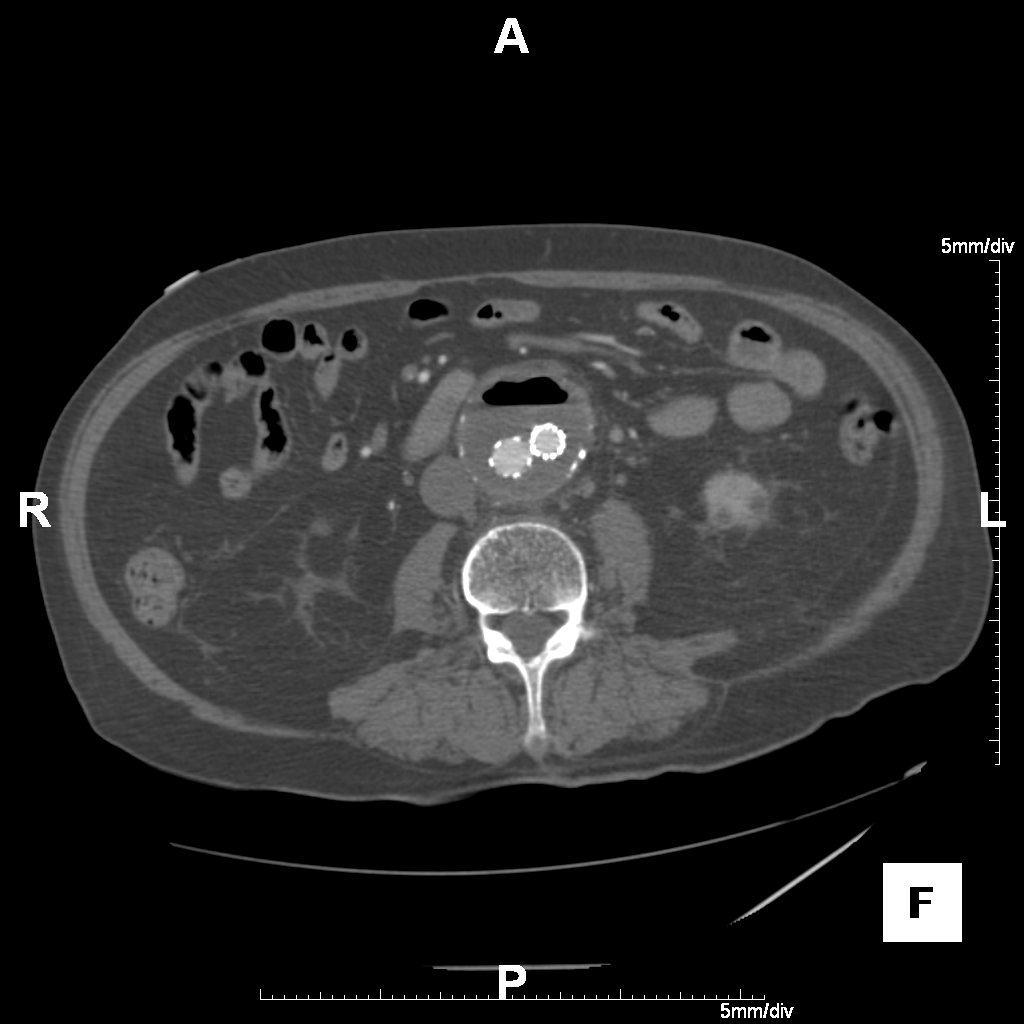
Back to Annual Meeting Posters

