Back to Annual Meeting Abstracts
Carotid Artery Stenting has Increased Risk of External Carotid Artery Occlusion Compared to Carotid Endarterectomy
Kevin A Brown1, Dina S Itum2, James G Reeves2, Yazan Duwayri2, Ravi Rajani2, Ravi K Veeraswamy2, Shipra Arya1, Atef Salam1, Thomas F Dodson2, Luke P Brewster1
1Emory University/ Atlanta VA Medical Center, Atlanta, GA;2Emory University, Atlanta, GA
Background: Carotid artery stenting (CAS) can offer advantages over carotid endarterectomy in certain patient populations, such as those with hostile necks. However, carotid endarterectomy (CEA) and CAS are fundamentally different. CAS routinely covers the the external carotid artery (ECA), and we hypothesize that this increases the risk of ECA occlusion. Since the ECA can be an important source of cerebral blood flow in cases of high-grade internal carotid artery stenosis or occlusion, ECA occlusion may be important to long-term cerebral perfusion. Furthermore, CAS causes disturbed flow into the ECA that likely promotes ECA stenosis and may contribute to in-stent restenosis (ISR). Our objective was to identify whether CAS increased the rate of external carotid artery occlusion, and whether ECA occlusion was associated with in-stent restenosis.
Methods: Patients undergoing CAS or CEA from February 2007-February 2012 with follow-up carotid ultrasounds in our system were identified from our institutional carotid database. There were a total of 312 CAS procedures (N=299 patients) and 344 CEA procedures (N=335) in this time period. For patients who had re-operation on the same carotid vessel (N=5 for CAS, N=5 for CEA), we used the last documented ultrasound prior to the date of re-operation. These ultrasounds were used to identify ECA occlusions and in-stent restenosis using consensus panel velocity criteria.
Results: There were 210 CAS patients with follow-up ultrasounds (67%), and there were 207 CEA patients with follow-up ultrasounds in our system (60%). The average follow-up of CAS was significantly shorter than the CEA group (0.7 years vs. 1.7 years; P<0.001), and CAS patients were more likely to take Plavix (97% vs. 35%; P<0.001). All other variables were similar between groups. We identified significantly more occluded ECA in the CAS (14) compared to the CEA (4) group (P=0.03). Additionally, 8 (57%) of 14 arteries with ECA occlusions had >50% ISR whereas 48 (26%) of 186 arteries without ECA occlusions had >50% ISR (P=0.02) (Fig. 1).
Conclusions: This is the first demonstration of increased ECA occlusion after CAS in the literature, but prior publications have identified increased external carotid stenosis. This finding was in spite of decreased follow-up time periods and increased use of Plavix in the CAS group, lending more validity to our results. A recent report identified disturbed flow in the ECA after CAS. This may be the biologic reason for these findings. The association of in-stent restenosis with ECA occlusion is also very interesting and warrants further investigation. We are currently determining whether ECA stenosis/occlusion occurs before, at the same time, or after in-stent restenosis. Establishing the timeline will be critical to identifying whether disturbed flow in the ECA has a causative role in in-stent restenosis. 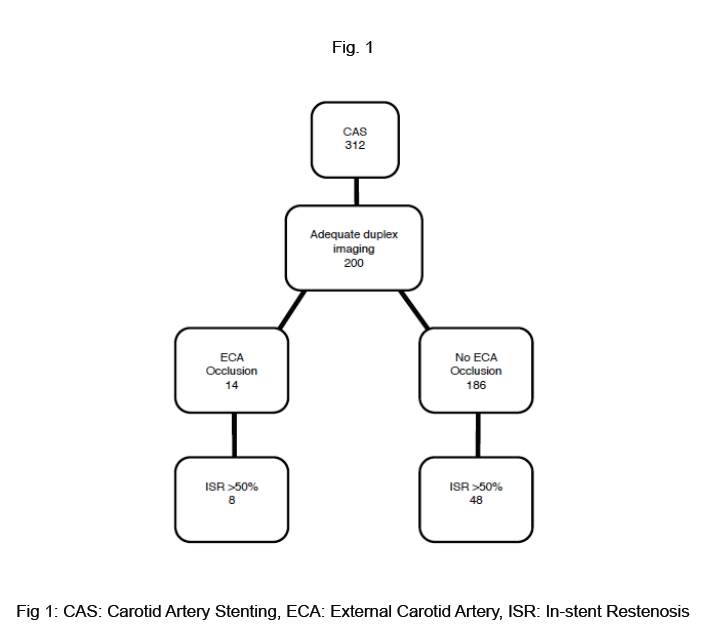
Back to Annual Meeting Abstracts
