Back to Annual Meeting Abstracts
EVAR Conversion for Type 1a Endoleak is not associated with Increased Morbidity or Mortality Compared to Primary Juxtarenal Aneurysm Repair
Michael M McNally, Salvatore T Scali, Robert J Feezor, Catherine K Chang, Alyson L Waterman, Scott A Berceli, Thomas S Huber, Adam W Beck
University of Florida, Gainesville, FL
Objectives: Due to concerns of increased morbidity and mortality with open surgical conversion (OSC) to manage Type 1a endoleaks after endovascular aortic repair (EVAR), reports of endoluminal salvage with fenestrated and/or chimney techniques have emerged. The purpose of this analysis was to determine outcomes of elective OSC and compare to primary juxtarenal open aortic aneurysm repair (POR).
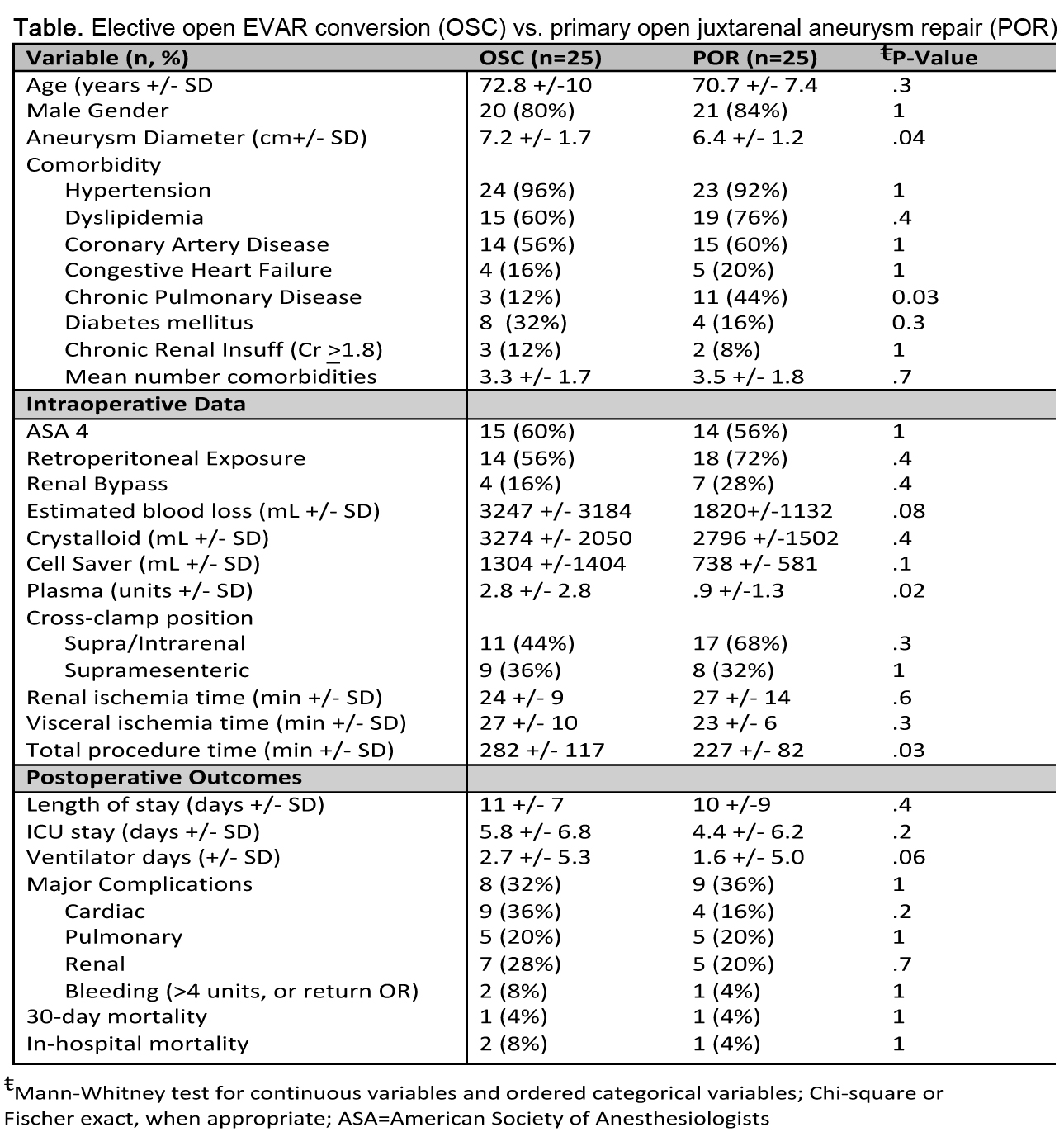
Methods: From 2002-2012, a total of 54 patients underwent EVAR conversion at median time of 26.8 months [interquartile range (IQR): 9.4, 54.6]. Indications included: endograft thrombosis (N=2, 3.8%), intraoperative EVAR failure (N=3, 5.5%), rupture (N=5, 9.2%), graft infection (N=6, 11.1%), and endoleak (N=38, 70.4%). Twenty-five patients underwent elective OSC for Type 1a endoleak and were compared with 25 anatomy and comorbidity-matched patients who underwent POR during the same time period. Primary end-points were 30-day and 1-year mortality. Secondary end-points included early complications, cross-clamp and procedure time, blood loss, and length of stay (LOS).
Results: Demographic and comorbidity data in the OSC and POR groups did not differ with the exception that POR patients presented with smaller aneurysm diameter and a higher rate of chronic obstructive pulmonary disease (Table). Compared to POR, OSC patients more frequently underwent a non-tube graft repair [OSC, N=6 (24%) vs. POR, N=20 (80%); P=.0002], required longer procedure times (P=.03), and received greater volumes of plasma transfusion (P=.02). With respect to all other measured outcomes, no significant differences were detected between the 2 groups (Table). The 30-day mortality was 4% in both groups (observed difference in rates = 0%, 95% CI for difference in mortality rates = [-14.0%, 14.0%], P=1). One-year survival was 83.3% in OSC and 90.5% in POR (observed difference in survival rates, POR-OSC = 7.2%, 95% CI for difference in rates = [-15.3%, 29.2%], P=.65).
Conclusions: Although there have been many advances in EVAR technology, the need for OSC persists, and may become more common as older generation devices fail. OSC can be technically challenging, but is not associated with increased morbidity or mortality when compared to POR. These results should be considered before pursuing complex endovascular remediation of EVAR failures.
Back to Annual Meeting Abstracts
