Back to Annual Meeting Abstracts
Brachiocephalic vein bypass with sternal reconstruction for symptomatic occlusion
Mark E O'Donnell, Dawn E Jaroszewski, Kathyrn Coan, Grant T Fankhauser, Richard J Fowl, William M Stone, Francis J Kazmier, Samuel R Money
Mayo Clinic, Phoenix, AZ
INTRODUCTION:Complications attributed to central venous stenosis and subsequent thrombosis are increasing in frequency and are most commonly associated with neointimal fibroplasia from venous access procedures as well as neoplastic,fibrotic,and traumatic pathologies.
METHODS:We present the successful venous bypass and thoracic wall reconstruction in a patient with chronic atypical symptomatology secondary to brachiocephalic vein occlusion from congenital thoracic dystrophy.
RESULTS:A fifty-eight year-old female presented with chronic holocephalic retro-orbital exertional headaches and an increased frequency of atypical symptomatology including intermittent vertigo,neck and shoulder discomfort combined with bulging of her left sided neck veins.She had no previous venous thromboembolic disease,venous access catheters or trauma.In December 2011,her headaches increased in frequency and severity and she also became syncopal on rising from a lying position.A contrast-enhanced CT angiogram identified significant narrowing of the left brachiocephalic vein between the sternum and descending thoracic aorta with concentric narrowing relating to either intraluminal thrombus or extrinsic compression.The anterior/posterior dimension between the sternum and spine was narrowed at less than 3.5 cm.Venography revealed a filling defect in left brachiocephalic vein and normal patency of the other great veins.She described consistent short-term relief after multiple percutaneous brachiocepahlic vein thrombolysis, angioplasty and stenting procedures performed at an outside institution.Repeat CT imaging suggested extrinsic compression of the previously inserted brachiocephalic stent.She was referred to vascular surgery where it was determined that operative decompression and venous bypass was warranted due to extrinsic pressure created between the sternum and aortic arch due to pectus excavatum.In order to expand the diameter of the upper chest,the upper manubrium,clavicle,sternum and ribs were released from scar tissue and the pectoralis muscles were elevated.Multiple transverse rib osteotomies were performed from the 1st to 3rd ribs at their sterno-costal junctions.The manubrium itself was depressed inward and a sternal osteotomy was necessary to elevate it.The left 1st and 2nd ribs were grossly deformed and were excised leaving a 3-4 cm chest wall hernia that was subsequently closed with XCM biologic tissue matrix®.The right great saphenous vein was endoscopically harvested and used to construct a spiral graft to bypass the left brachiocephalic vein between the junction of the left internal jugular and brachiocephalic vein to the SVC.Intra-operative duplex assessment confirmed good flow in the vein bypass.The chest wall was reconstructed utilizing titanium plating and FiberWire™ to reattach the ribs and manubrium to the elevated sternum.After the manubrium was elevated to a more anterior position,a significant deficiency in clavicle length was present, especially on the left side.Bilateral autologous semitendinosus grafting of clavicles to manubrium was performed(Figure 1).Post-operatively,the patient had an uneventful recovery and remains well seven-months later.
CONCLUSIONS:Although acute central vein obstruction warrants urgent intervention, treatment of chronic occlusions remain less descript.Despite reported equivocal results between operative intervention and repeated angioplasty,open brachiocephalic vein bypass is suggested for longer term relief in patients with any etiological anatomical compression. 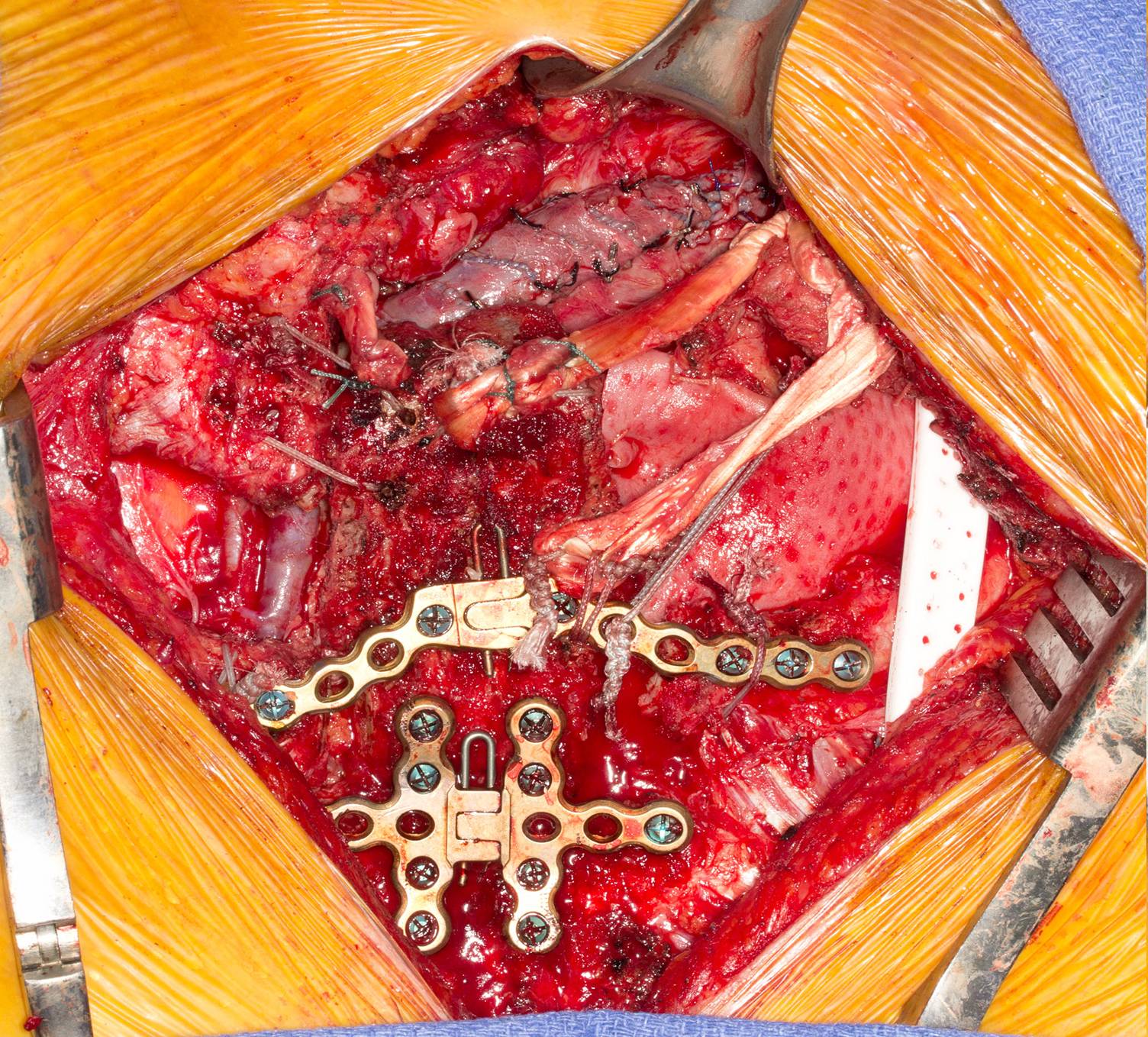
Back to Annual Meeting Abstracts
