Back to 2015 Annual Meeting Abstracts
Routine Postoperative Carotid Duplex Ultrasound Surveillance after Carotid Endarterectomy
Ali F AbuRahma, Mohit Srivastava, Zachary AbuRahma, Will Jackson, Patrick A Stone, Jason Green, L Scott Dean, Albeir Y Mousa
West Virginia University, Charleston, WV
INTRODUCTION: Several studies have reported on the role of postoperative duplex ultrasound surveillance after carotid endarterectomy (CEA) with varying results. Most of these studies had a small sample size and/or didn’t analyze cost effectiveness. Therefore, there is no consensus regarding its usefulness and whether or not it is cost effective.
METHODS:
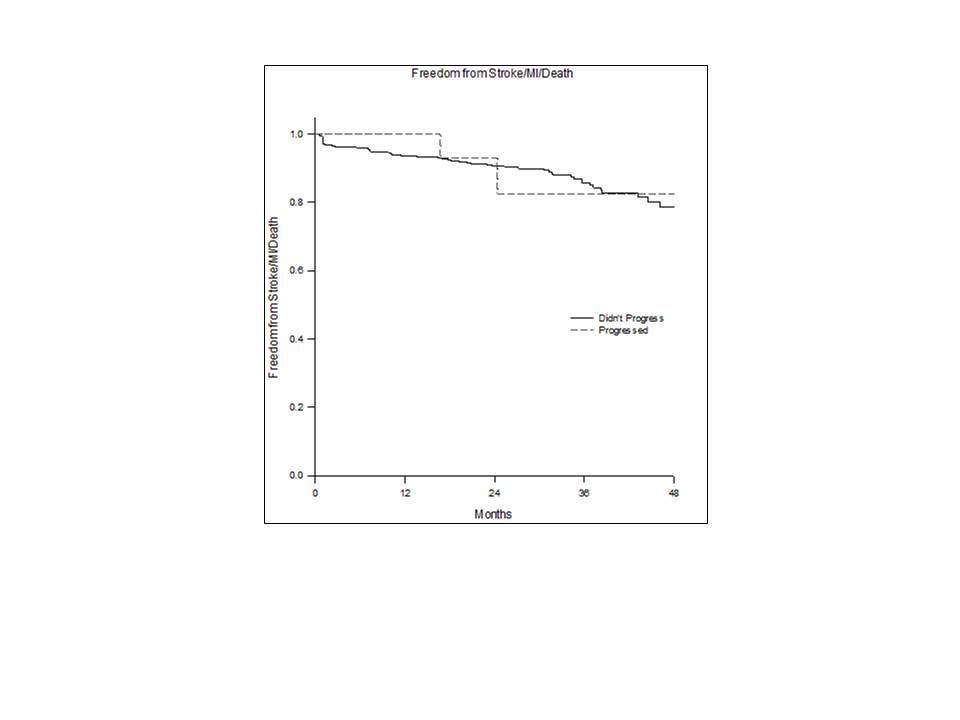
489/501 CEA patients with patch closure were analyzed. All patients had immediate postoperative duplex ultrasound and were routinely followed both clinically and with duplex ultrasound at regular intervals of 1, 6, 12 months, and every 12 months thereafter. A Kaplan Meier analysis was used to estimate the rate of ≥50% and ≥80% post CEA restenosis over time and the time frame of progression from normal to ≥50% or ≥80% restenosis. The cost of post CEA duplex surveillance was also estimated.
RESULTS:
Overall, 489 patients with a mean age of 68.5 years were analyzed. Ten of these had residual postoperative ≥50% stenosis and 37 did not undergo a second duplex ultrasound and, therefore, were not included in the final analysis. The mean follow-up was 20.4 months (range: 1-63 months) with a mean number of duplex ultrasounds of 3.6 (range 1-7). Eleven of 397 patients (2.8%) with a normal immediate postoperative duplex ultrasound versus 4/45 (8.9%) with mild stenosis on immediate postoperative duplex ultrasound progressed to ≥50% restenosis (p=0.055). Overall, 15 patients (3.1%) had ≥50% restenosis: nine with 50-<80%, and four with 80-99% (two of these had carotid artery stenting reintervention), and two had late carotid occlusion. All of these were asymptomatic, except for one who had a transient ischemic attack. The mean time to ≥50%-<80% restenosis was 14.7 months versus 19.8 months for ≥80% restenosis after the CEA. Freedom from ≥50% and ≥80% restenosis rates were 98%, 96%, 94%, 94%, 94%, and 99%, 98%, 97%, 97%, and 97% at 1, 2, 3, 4, and 5 years, respectively (Figure 1). Freedom from MI/stroke/deaths was not significantly different between patients with and without restenosis (100%, 93%, 83%, and 83% versus 94%, 91%, 86%, and 79% at 1, 2, 3, and 4 years, respectively, p=0.951, Figure 2). The estimated cost of this surveillance was 3.6 x 489 (number of CEAs) x $800 (charge for carotid duplex ultrasound), which equals $1,408,320, to detect only four patients with ≥80%-99% restenosis who may have been potential candidates for reintervention.
CONCLUSIONS:
This study confirms that routine postoperative duplex ultrasound surveillance after CEA with patch closure is not necessary and/or cost effective, particularly if the immediate postoperative duplex ultrasound was normal or had minimal disease.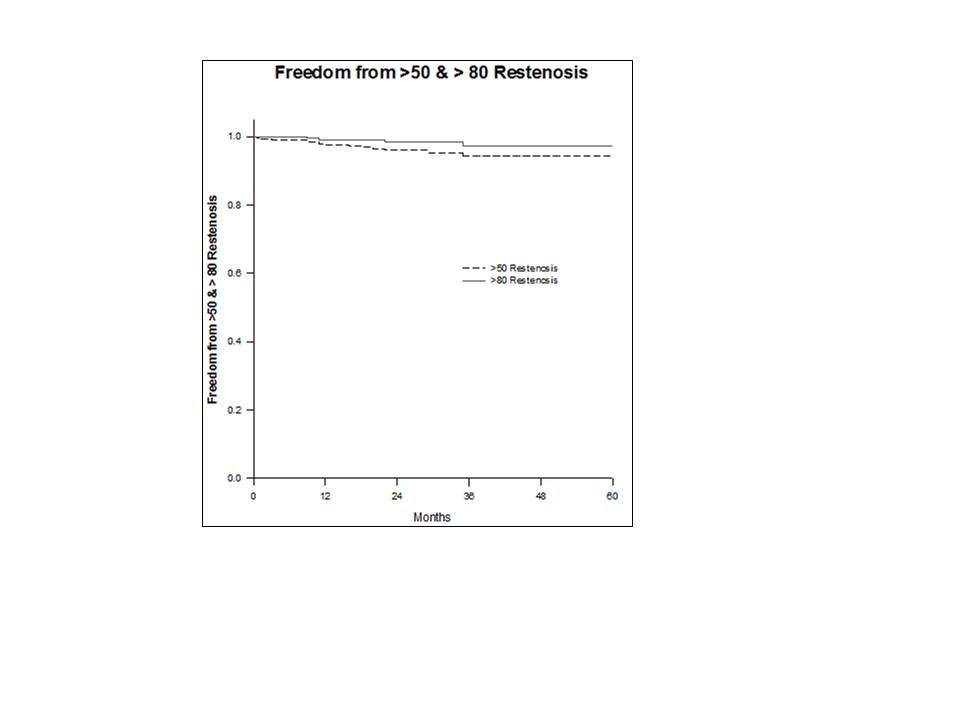
Back to 2015 Annual Meeting Abstracts
