Back to 2015 Annual Meeting Abstracts
Primary Stent Placement Improves Patency After Endovascular Treatment of Hepatic Artery Stenosis Following Liver Transplantation
Linda Le, William Terral, Nicolas Zea, Hernan A. Bazan, Taylor A. Smith, George E. Loss, Edward Bluth, W. Charles Sternbergh, III
Ochsner Clinic, New Orleans, LA
Objective: Significant hepatic artery stenosis (HAS) after orthotopic liver transplantation (OLT) can lead to thrombosis with subsequent liver failure in 30% of patients. While operative intervention or re-transplantation has been the traditional solution, endovascular therapy has emerged as a less-invasive treatment strategy. Prior smaller studies have been conflicting in the relative efficacy of angioplasty (PTA) versus primary stent placement for HAS.
Methods: This was a single center retrospective review of all endovascular interventions for HAS after OLT over a 54-month period (August 2009-December 2013). Patients with ultrasound evidence of severe HAS (peak systolic velocity > 400 cm/sec, resistive index of <0.5, tardus parvus spectral abnormalities) underwent endovascular treatment with primary stent placement or PTA. Outcomes calculated were technical success, primary and primary assisted patency rates, re-interventions, and complications.
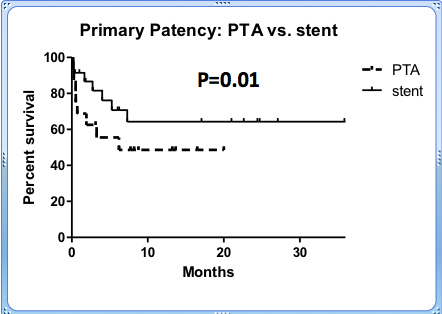
Results: Sixty-two interventions for HAS were performed in 42 patients with a mean follow-up of 19.1 ± 15.2 months. During the study period, the rate of treated HAS was 6.4% (42/654). Primary technical success was achieved in 95% (59/62) of cases. Initial treatment was with PTA alone (n=16) or primary stent (n=26). Primary patency rates after initial stent placement were 91%, 81.3%, 77%, and 77% at 1,6,12, and 24 months, respectively, significantly better (P=0.01) when compared to initial PTA (68.8%, 57.1%, 44%) see Figure. There were 20 re-interventions in 14 patients (8 stents, 6 PTA) for recurrent HAS. The time to initial re-intervention in patients with PTA alone vs. initial stent was 51 and 105.8 days, respectively. 75% of re-interventions required stent placement of which 5 drug-eluting stents were placed. Overall primary patency rates (Kaplan-Meier) were 82%, 70%, 63%, and 50% at 1,6,12, and 24 months, respectively. Overall primary-assisted patency was 96% and 93% at 12 and 24 months. Major complications were one arterial rupture treated endovascularly, and two hepatic artery dissections. Long-term risk of HAT in the entire patient cohort was 4.8%.
Conclusions: In this series, which represents the largest reported cohort of endovascular interventions for HAS to date, we demonstrate that HAS after liver transplantation can be treated endovascularly with high initial technical success and excellent primary-assisted patency. Initial stent placement significantly decreased the need for re-intervention. Avoidance of hepatic artery thrombosis (HAT) is possible in >95% of patients with endovascular treatment and close follow-up.
Back to 2015 Annual Meeting Abstracts
