Back to 2015 Annual Meeting Abstracts
Validated Prediction of Groin Infection after Revascularization Procedures
Kyla M Bennett, Howard Levinson, John E Scarborough, Cynthia K Shortell
Duke University Medical Center, Durham, NC
Background: Groin wound infection is a costly and morbid event after lower extremity revascularization. To date, a comprehensive and validated method for identifying patients who are at greatest risk for this complication, and who might therefore benefit from prophylactic muscle flap coverage of their initial groin incision, has yet to be developed.
Methods: Our retrospective analysis included all patients at a single institution who underwent lower extremity revascularization using a groin incision from 2009 through 2012. Patients were randomly divided into two groups (matched for operative year and surgeon): a PILOT group which was used to develop a predictive model for our primary outcome, and a VALIDATION group which was used to test that model. The primary outcome for our analysis was groin wound infection requiring operative intervention. Potential predictor variables included patient age, sex, year of operation, previous groin incision, use of thrombolytic agents, concomitant amputation, body mass index (BMI), smoking status, diabetes mellitus, end-stage renal disease, malnutrition, preoperative wound, type of conduit, level of distal target vessel, and emergency status of the index operation. Best fit model selection methods were used to evaluate all possible combinations, interactions, and transformation of potential predictor variables from the PILOT patient group. The resulting model with the lowest Akaike Information Criterion was then selected for testing using the VALIDATION patient group. A user-friendly computer program was then developed which utilizes this model to predict an individual patient's risk of operative groin wound infection.
Results: A total of 284 patients who underwent lower extremity revascularization procedures were included in our study (141 in the PILOT group, 144 in the VALIDATION group). 17 (12.1%) of patients from the PILOT group developed groin incision infection that required operation. The predictive model that was developed from this group yielded the following independent predictors of operative groin wound infection: previous groin incision, female gender, BMI, ESRD, malnutrition, and urgent/emergency operation status. The c-index of the resulting model was 0.845, and resulted in a correct classification of 88.6% of patients. Subsequent testing in the VALIDATION group (13.9% of whom sustained an operative groin wound infection) yielded an accuracy of 86.1% for our predictive model. We therefore developed a user-friendly computer program (which will be publicly accessible) which can be used to calculate an individual patient's risk of developing operative groin wound infection after lower extremity revascularization (see Figure 1).
Conclusion: Our study is the first known attempt to develop and internally validate a statistical model that will accurately predict those patients who are likely to sustain an operative groin wound infection after lower extremity revascularization.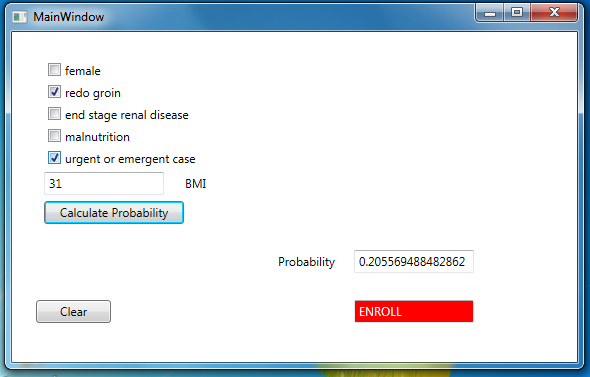
Back to 2015 Annual Meeting Abstracts
