Back to 2015 Annual Meeting Abstracts
Biochemical Markers in Patients with Peripheral Vascular Disease: Comparison between Endovascular and Open Reconstructions
Patrick A Stone1, John E Campbell1, Stephanie N Thompson2, David Williams1, Zachary AbuRahma1, Luke Grome1, Haley Schlarb1, Molly John1, Ali F AbuRahma1
1West Virginia University/Charleston Area Medical Center, Charleston, WV;2CAMC Health Education and Research Institute, Charleston, WV
INTRODUCTION: Previously our group has reported on the preoperative markers, high-sensitivity C-reactive protein (hsCRP) and B-type natriuretic peptide (BNP), and their ability to predict future major adverse limb events (MALE) and major adverse cardiovascular events (MACE) following lower extremity endovascular interventions. Others have reported on the predictive power of these biomarkers for adverse outcomes in either endovascular cohorts or open surgical reconstructions. No literature currently addresses the use of these biomarkers while comparing revascularization strategies or while examining autologous and prosthetic reconstructions in surgical bypasses.
METHODS: We retrospectively examined patients who underwent elective endovascular intervention or open surgical reconstruction for lower extremity peripheral arterial occlusive disease between the dates of January 1, 2007 and December 31, 2013. All procedures were performed by a single operator. Patients had pre-procedure levels of hsCRP and BNP and post-procedure imaging (ankle-brachial index, duplex ultrasound imaging or contrast angiography). Examined outcomes included MALE (composite endpoint of target vessel revascularization, limb amputation, or disease progression) and MACE (stroke, myocardial infarction, or death) occurring by 24 months. The relationship between baseline hsCRP and BNP levels and to time to the MALE and MACE was examined by univariate and multivariate Cox proportional hazard regression analyses.
RESULTS: A total of 245 limbs in 200 patients were included in analysis (median age [interquartile range]: 63 [53-71] years) with 156 limbs receiving endovascular revascularization and 89 limbs receiving surgical reconstruction. The surgical cohort was composed of a greater proportion of: males (62 vs. 42%, p=0.01), limbs with critical limb ischemia (60 vs. 17%, p < 0.01), and outflow procedures (82 vs. 39%, p < 0.01) compared to the endovascular cohort. Pre-procedural levels of hsCRP and BNP did not differ between surgical and endovascular treated limbs (hsCRP: 0.57 [0.26-1.18] vs. 0.43 [0.22-0.96] mg/dL, p = 0.21, BNP: 43 [18-112] vs. 44 [18-82] pg/mL, p = 0.66, surgical vs. endovascular cohorts, respectively). When endovascular treated limbs were examined in isolation, multivariate analysis demonstrated that higher hsCRP levels significantly associated with MALE (hazard ratio (HR): 1.2[1.0-1.4] p = 0.02). In surgical reconstructions, neither BNP nor hsCRP associated with MALE, however the use of a vein bypass conduit (vs. prosthetic reconstruction) significantly predicated MALE (HR: 3.5[1.6-7.6], p < 0.01). hsCRP failed to associated with MACE in either endovascular or surgical treated limbs. However, elevated BNP levels associated with MACE in the surgical cohort (HR: 1.03[1.01-1.04] p < 0.01) but not in those receiving endovascular intervention.
CONCLUSIONS: Elevated hsCRP levels predicted inferior results in endovascular reconstructions while elevated BNP levels associated with impaired long term survival in patients with surgical revascularizations. Additional studies should use biochemical markers to further stratify outcomes following both types of vascular interventions as a means to elucidate how biomarkers can best assist clinical decision-making for outcome improvement. 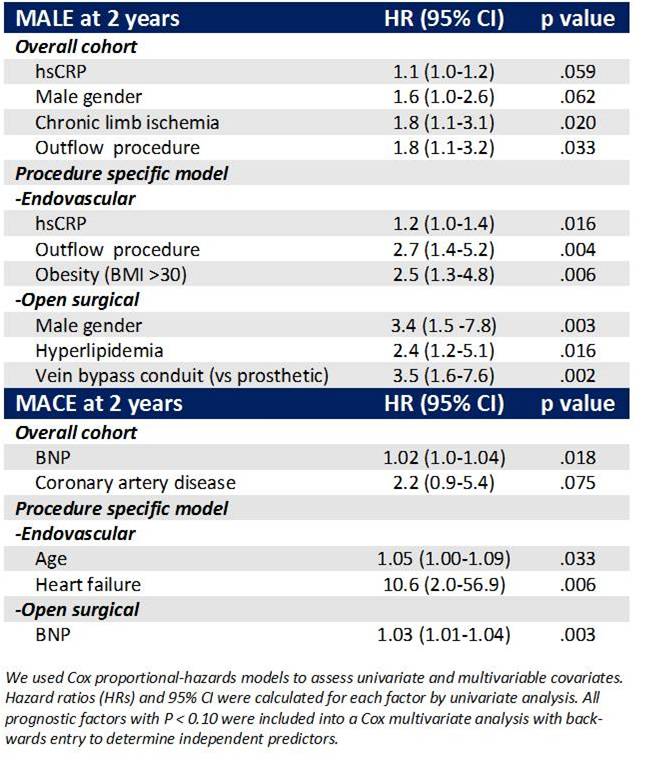
Back to 2015 Annual Meeting Abstracts
