Back to 2015 Annual Meeting Posters
A comparison of the short-term outcomes of elective inflow revascularization for claudicants
Arin L Madenci1, C Keith Ozaki1, Naren Gupta2, Joseph D Raffetto2, Michael Belkin1, James T McPhee2
1Brigham and Women's Hospital, Boston, MA;2VA Boston Healthcare System, Boston, MA
INTRODUCTION: We compare the contemporary early post-operative morbidity and mortality rates of aortofemoral bypass (AFB) and inflow procedures for claudication.
METHODS: We identified claudicants who underwent elective AFB (bilateral or unilateral) or non-AFB (NAFB) inflow procedures (isolated common femoral artery [CFA] endarterectomy; femoral-femoral bypass; or bilateral/unilateral axillo-femoral or ilio-femoral bypass) in the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) 2005-2011 databases. Follow-up was 30 days post-operatively. Stent placement was not routinely captured over this interval. Patients undergoing AFB and NAFB were propensity score matched on baseline characteristics. The primary outcome was 30-day post-operative mortality. Secondary outcomes include major cardiac, respiratory, renal, infectious, and other complications.
RESULTS: A total of 2367 patients were surgically treated for claudication (664 with AFB and 1703 with NABF). Baseline characteristics of the unmatched and matched cohorts are shown in Table. Factors associated with use of AFB vs. NABF included female gender (adjusted odds ratio [OR]=1.81, 95% confidence interval [CI]=1.46-2.26, P<0.0001); recent tobacco use (OR=2.17, 95% CI=1.72-2.37, P<0.0001), diabetes (OR=0.76, 95% CI=0.58-0.99, P=0.0426) and pre-operative anemia (OR=0.76, 95% CI=0.60-0.97, P=0.0243). In the analysis of 1072 propensity score matched patients (536 pairs), the thirty-day mortality rate was lower for NAFB compared to AFB patients (0.0%, n=0 vs. 2.2%, n=12, P=0.0005). Additionally, NAFB patients had significantly lower rates of cardiac (0.2%, n=1 vs. 2.4%, n=13, P=0.0012), respiratory (0.7%, n=4 vs. 10.5%, n=56, P<0.0001), renal (0.2%, n=1 vs. 2.2%, n=12, P=0.0021), wound (1.7%, n=9 vs. 5.0%, n=27, P=0.0023), and septic (0.6%, n=3 vs. 4.9%, n=26, P<0.0001) complications and returned to the OR less frequently (4.1%, n=22 vs. 11.4%, n=61, P<0.0001). Rates of VTE, nerve injury, and graft failure were similar. Outcomes are displayed in Figure. Post-operative length of stay was longer in the AFB group (median [interquartile range], 6 [5-8] vs. 2 [2-3] days, P<0.0001).
CONCLUSIONS: In a propensity score matched analysis of similar patient groups in this national, multi-institutional sample, AFB was associated with higher rates of mortality and major complications than other inflow procedures. Multi-institutional long-term follow-up data would be valuable to determine if the benefit of the less-invasive nature of NAFB inflow procedures is tempered by their potential for decreased durability compared with AFB. 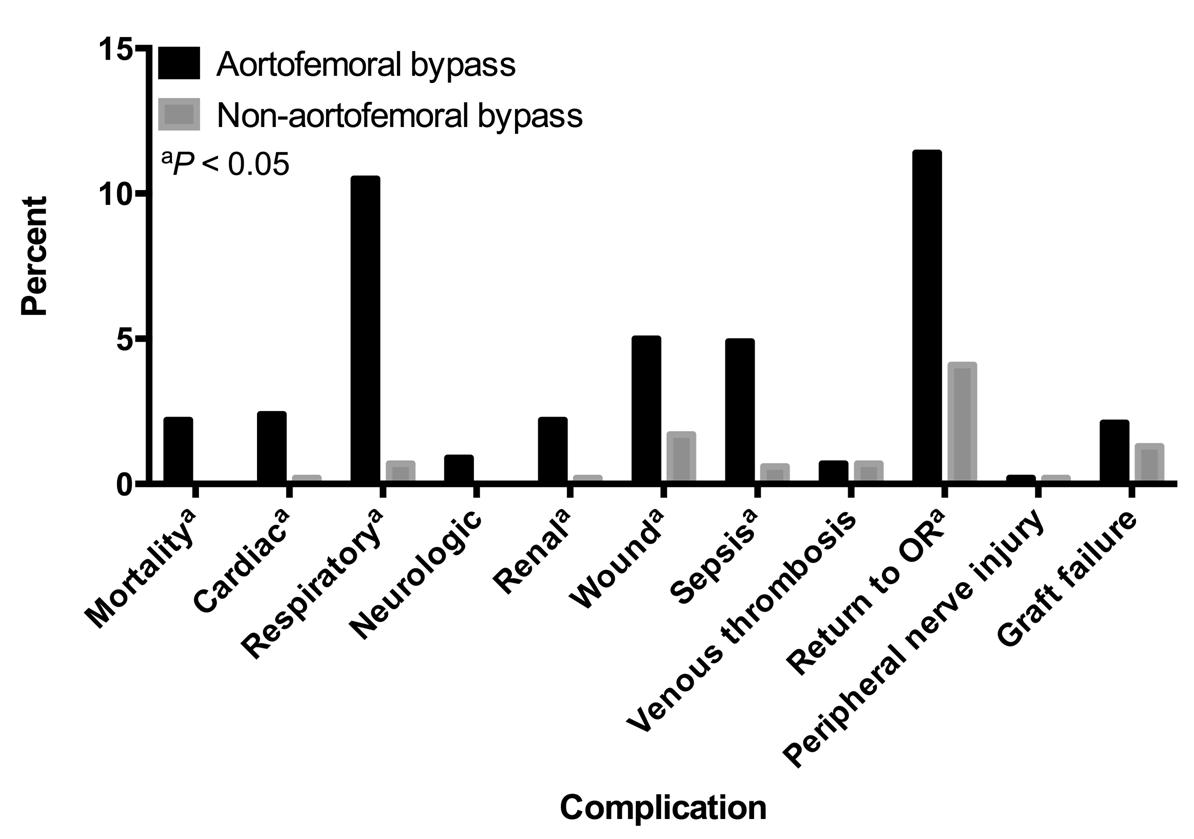
| Overall Series (N=2367) | Propensity Score-Matched Pairs (N=1072) | |||||
| Variable | AFB | NAFB | P | AFB | NAFB | P |
| N (%) | 664 (28.1) | 1703 (71.9) | 536 (50.0) | 536 (50.0) | ||
| Age≥65 | 238 (35.8) | 994 (58.4) | <0.0001 | 184 (34.3) | 187 (36.4) | 0.4822 |
| Female | 300 (45.2) | 579 (34.1) | <0.0001 | 244 (45.5) | 234 (43.7) | 0.5489 |
| Prior MI | 9 (1.5) | 21 (1.4) | 0.8557 | 7 (1.3) | 8 (1.5) | 0.7948 |
| Prior cardiac stent | 116 (18.9) | 323 (21.0) | 0.2774 | 106 (19.8) | 98 (18.3) | 0.5336 |
| Tobacco use | 474 (71.4) | 782 (45.9) | <0.0001 | 388 (72.4) | 392 (72.9) | 0.8371 |
| Severe COPD | 106 (16.0) | 246 (14.5) | 0.3508 | 81 (15.1) | 78 (14.5) | 0.7966 |
| BMI≥30 | 171 (25.8) | 501 (29.6) | 0.0638 | 137 (25.6) | 149 (27.8) | 0.4073 |
Back to 2015 Annual Meeting Posters
