Predictors of Outcome in Infrainguinal Bypass for Trauma
Hunter M Ray, Harleen K Sandhu, Charles C Miller, Edmundo Dipasupil, Rana O Afifi, Ali Azizzadeh, Kristofer Charlton-Ouw
The University of Texas Medical School at Houston, Houston, TX
Background:
Trauma remains a leading cause of morbidity and mortality worldwide, with vascular injuries present in 1-2% and with the majority of injuries occurring to the extremities. This study aims to determine predictors of poor outcome in infrainguinal bypasses performed for traumatic arterial injury.
Methods:
Patients admitted between September 1999 and July 2015 who underwent infrainguinal arterial bypass for trauma at a single level one trauma center were included for analysis. Poor outcome was defined as a composite comprised of thrombosis leading to graft abandonment, reoperation, major amputation or death. Data were analyzed by stratified Kaplan-Meier and multiple Cox regression analysis using SAS v9.4 (SAS Institute, Cary, NC).
Results:
During the study period, 108 patients had infrainguinal arterial bypass for traumatic arterial injury, composed of 45 end-to-side and 63 interposition bypasses. Mean age was 35±17 years-old; 17/108 (16%) were female; median Injury Severity Score (ISS) was 12 (IQR 9-18); admission glomerular filtration rate (GFR) was 77.5 (IQR 59-92); median Mangled Extremity Severity Score (MESS) was 6 (IQR 5-7); median injury-to-surgery time was 5.1 hours (IQR 2-24); 39/108 (36%) had blunt injury; 30/108 (28%) had crush injury; 39/108 (36%) had motor vehicle collision (MVC); 10/108 (10%) had diabetes mellitus (DM); and 76/108 (70%) had an infrageniculate target for bypass.
Univariate risk factors for poor outcome include age >40 years (48% vs 21%, p<0.01); MESS>7 (51% vs 14%, p<0.01); blunt mechanism (39% vs 15%, p<0.01); diabetes (70% vs 27%, p<0.01); and infrageniculate target vessel (37% vs 16%, p<0.03). Popliteal artery injury (38% vs 21%, p<0.06) and concomitant orthopedic injuries (35% vs 17%, p<0.06) had worse outcomes, yet were not statistically significant. Baseline renal function, injury-to-surgery time, surgeon’s specialty, and associated venous injuries were not significantly predictive of poor outcome. MESS was strongly predictive of poor outcome, with probability rising as high as 95% when MESS reached 12 (Figure 1). A MESS score >7 was 73% sensitive and 70% specific to predict poor outcomes.
Age (OR 1.03/year, p<0.04) and MESS >7 (OR 3.8, p<0.02) were persistent predictors of poor outcome in multivariable analysis. In stratified analysis, interposition grafts fared worse only in penetrating injuries with composite poor outcome in 0/13 (0%) in end-to-side vs. 6/26 (23%) in interposition bypass (RR 1.3; 95% CI 1.1-1.6; p<0.03).
Conclusion:
Poor outcome in infrainguinal bypass for trauma is predicted by age >40 years, MESS>7, blunt mechanism of injury, infrageniculate target as well as history of DM. Interestingly, interposition bypasses had worse outcomes compared to end-to-side bypasses only in penetrating injures.
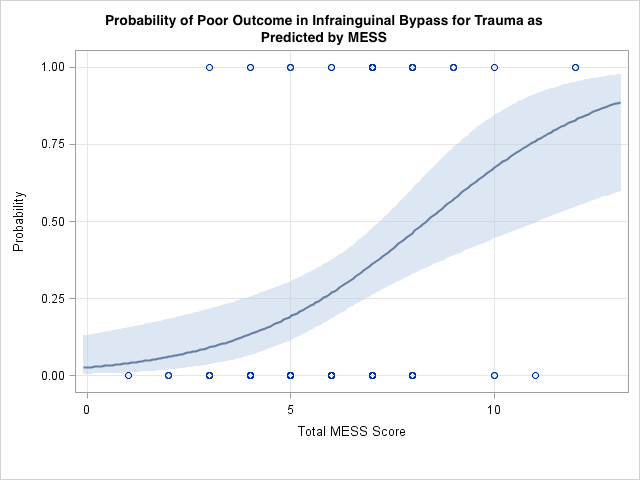
Figure 1: Logistic Regression plot demonstrating poor predicted outcome with increasing Mangled Extremity Severity Score (MESS) with 95% probability of poor outcome predicted when MESS reached 12.
Back to 2018 Abstracts




