Warm ischemia time decreases primary patency of cryopreserved conduits in patients undergoing lower extremity bypass
J. Michael Cullen, J. Hunter Mehaffey, Robert B Hawkins, Vikram Gupta, Rishi Roy, William P Robinson, III, Margaret C Tracci, Kenneth J Cherry, John A Kern, Gilbert R Upchurch, Jr.
University of Virginia, Charlottesville, VA
BACKGROUND
Autologous vein is the preferred conduit for lower extremity bypass in patients with peripheral arterial disease (PAD) due to superior patency. However, autologous vein is often unavailable because it has been previously harvested, or is of inadequate caliber for a successful bypass. Cryopreserved veins and arteries are being increasingly used in these situations, although the literature reports patency rates inferior to both autologous vein and synthetic materials. Consequently, some authors have proposed that cryopreserved conduits should be used only as a last resort, or only for critical limb ischemia. Extensive literature demonstrates that numerous cadaveric donor characteristics impact clinical outcomes in organ allotransplantation, but little is known about how donor characteristics impact vascular allotransplantation. Currently, variables impacting the patency of cryopreserved conduits remain an understudied area of clinical importance. The purpose of this study was to examine the risk-adjusted impact of cadaveric donor, patient, and operative characteristics on primary patency in patients undergoing lower extremity bypass. We hypothesized that increased warm ischemia times (WIT) would negatively impact the primary patency of these bypass grafts.
METHODS and MATERIALS
Clinical Data
Clinical data for all patients who received a cryopreserved femoral artery, vein, or saphenous vein for lower extremity bypass for symptomatic PAD at a single center institution from 2010-2016 were included for analysis. Patient data was obtained from the institutional Clinical Data Repository (CDR) and chart review. Allograft donor blood type and WIT were provided by the tissue processing organization. This study was approved by the Institutional Review Board with a waiver of consent due to its retrospective nature.
Variable definitions and outcomes
This study’s primary outcomes were primary patency and patient survival. Primary patency was defined according to the recommended reporting standards as detailed by Rutherford et al. In short, the graft is considered to have lost primary patency with interruption of flow by any means. Loss of primary patency was determined by objective testing including duplex ultrasound, computed tomography, and angiogram; physical examination was not used for this assessment. Preoperative variables of interest were comorbidities, donor blood type, WIT, type of bypass, and the use of arterial or venous allograft. Below the knee bypasses were classified as those with any infrageniculate target, including femoral-below-the-knee-popliteal and distal bypasses. Distal bypasses were classified as those to the tibioperoneal trunk and anterior or posterior tibial artery.
Statistical Analysis
Continuous variables are presented as mean ± standard deviation and categorical variables as count (percent). Patients were stratified by primary patency status for univariate analysis, either t-test or chi-square as appropriate. Additionally, the impact of preoperative variables on time to loss of primary patency was evaluated using Kaplan-Meier analysis. A Cox proportional hazards model was used to determine risk-adjusted associations. All statistical analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC).
RESULTS
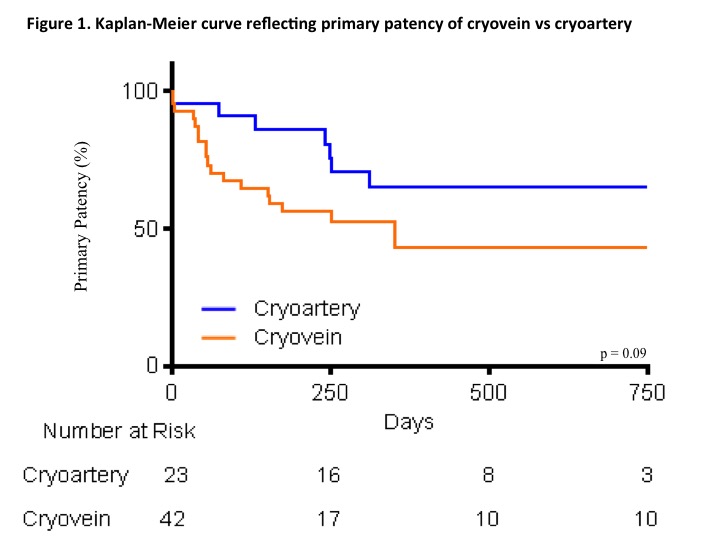
A total of 60 patients with PAD underwent lower extremity bypass with 65 cryopreserved conduits during the study period. Primary patency at 1 year was 26.2%. Types of bypass were categorized into axillary-femoral (n=5), iliac-femoral (n=5), femoral-femoral (n=11), femoral-popliteal (n=11), popliteal-distal (n=4), and femoral-distal (n=29). Average survival was 581.5 ± 559.7 days. The most common surgical indication was critical limb ischemia (64.6%, p < 0.01). Twenty-three cryopreserved arteries and 42 cryopreserved veins were implanted. Duration of primary patency was 354.0 ± 241.3 days for the cryopreserved arteries and 358.2 ± 481.1 days for the veins (p = 0.11). Of the 6 arterial conduits used for a below the knee bypass, duration of primary patency was 212.4 ± 103.8 days. Of the 36 venous conduits used for below the knee bypass, duration of primary patency was 366.6 ± 465 days. By univariate analysis there were no significant differences in patient characteristics between those who lost primary patency and those who did not. There was no statistical difference between donor variables: arterial or venous conduit, conduit diameter, WIT, blood type, Rhesus immunization, or seromatch. Donor blood type was not available for 9 cases. Although not statistically significant, it appeared that tobacco use was clinically significant, as 69% of failed primary patency patients were current smokers whereas only 49% of those with continued patency were smokers (p = 0.10). There was no statistically significant difference in primary patency between type of bypass or infrageniculate target. Time to loss of primary patency using Kaplan-Meier analysis demonstrates that cryopreserved femoral artery conduits were more likely to remain patent and this trended toward significance (p = 0.09). Overall, the mean duration of primary patency with a venous conduit was 223 days, and the mean duration of primary patency with an arterial conduit was 267 days. After adjusting for indication, comorbid conditions such as kidney disease, diabetes and tobacco usage, and type of bypass, risk-adjusted primary patency independently decreased with each hourly increase in WIT (Hazard ratio [HR] 1.1; p = 0.02). Femoral to femoral artery bypasses had the highest rate of primary patency (HR 0.01; p = 0.01), and popliteal-distal bypass had a much higher loss of patency (HR 5.3; p = 0.07). Cryopreserved artery compared to cryopreserved vein did not independently predict patency in this population (HR 0.7; p = 0.60).
CONCLUSION
The present study reports the impact of cadaveric donor characteristics on the primary patency of cryopreserved vascular conduits used for lower extremity bypass. These data showed that primary patency decreased as WITs increased (HR 1.1; p = 0.02). Popliteal-distal bypasses had the worst primary patency, and bypasses in the femoral-femoral position had superior patency among the study population. These results provide additional insight into using cryopreserved conduits for these procedures. Overall primary patency at 1 year in the present study was 26.1%, and this is analogous to other reports. In a series of 35 patients, Walker et al reported 28% patency in the same interval. The largest series to date, including 177 patients and 240 conduits, by Farber et al had a similar rate of 30% at 12 months. The findings of no significant increase in loss of primary patency with differing donor blood types are consistent with that of Walker et al. However, other studies have found outcomes affected by ABO incompatibility. O’Banion et al found that ABO incompatibility was a significant risk factor for 30-day graft failure. Zehr et al reported that only 6 of 20 non-compatible grafts offered limb salvage. In other studies, centers seromatched all donor veins to recipients, but did not find a difference between different donor blood type or Rh immunization and patency. Cryopreserved femoral arteries are much more robust tissue than saphenous vein, and the robust patency of arterial conduits compared with venous conduits in cardiac surgery is well known. Only a few studies have reported outcomes with cryopreserved arterial conduits, and these found a high rate of degeneration and loss of patency. In the current study, there was no significant difference in patency between artery and vein, even with below-the-knee bypass. A limitation of this study is that it may have been underpowered to demonstrate statistical significance. Duration of ischemia time is a known variable affecting outcomes in organ allotransplantation. Many techniques are currently used in clinical practice to condition organs that have been subject to extended ischemia times in order to improve outcomes. Considering this, it may not be surprising that longer ischemia times could impact graft patency from femoral arteries and saphenous veins harvested from cadaveric donors. However, this has not been previously reported in the vascular surgery literature and is a unique finding of the current analysis. Further studies should continue to evaluate the impact of ischemia time on patency in order to determine if this factor will continue to have a role in graft patency and survival. Limitations of the present study include its retrospective nature with inherent risk of selection bias, as well as the limited number of patients (n = 60). Clinical decisions should not be made based on the results of a single study with limited subject numbers. Further, the reported observations are merely associations between donor characteristics and primary patency; this does not imply a direct cause and effect relationship. In addition, the conduit diameters reported herein are from the product insert schematic; it is possible that intraoperative trimming could have affected the accuracy of these measurements. The current results indicate that increased WITs are associated with increased risk-adjusted loss of primary patency of lower extremity bypasses and reflect the outcomes of a single institution cohort of vascular surgery patients. Larger future analyses related to the impact of donor characteristics on cryopreserved conduits are warranted due to the potential to significantly impact patient outcomes.
Table 1. Operative and donor characteristics stratified by primary patency
| Lost Primary Patency | Ongoing Primary Patency | p-value | ||
| Critical limb ischemia | 18 (69.2%) | 24 (61.5%) | 0.87 | |
| Aneurysm | 3 (11.5%) | 7 (18.0%) | 0.87 | |
| Claudication | 2 (7.7%) | 4 (10.3%) | 0.87 | |
| Infected graft | 3 (11.5%) | 4 (10.3%) | 0.87 | |
| Axillary-femorala | 2 (7.7%) | 3 (7.7%) | 0.19 | |
| Iliac-femorala | 3 (11.5%) | 2 (5.1%) | 0.19 | |
| Femoral-femorala | 1 (3.9%) | 10 (25.6%) | 0.19 | |
| Femoral-popliteala | 5 (19.2%) | 6 (15.4%) | 0.19 | |
| Femoral-distala | 12 (46.2%) | 17 (43.6%) | 0.19 | |
| Popliteal-distala | 3 (11.5%) | 1 (2.6%) | 0.19 | |
| Cryoartery | 7 (26.9%) | 16 (41.0%) | 0.24 | |
| Infrageniculate | 18 (69.2%) | 24 (61.5%) | 0.52 | |
| Aspirin | 24 (92.3%) | 31 (79.5%) | 0.16 | |
| Dual antiplatelet therapy | 14 (53.9%) | 9 (23.1%) | 0.01 | |
| Donor A | 9 (40.9%) | 15 (44.1%) | 0.97 | |
| Donor B | 4 (18.2%) | 6 (17.7%) | 0.97 | |
| Donor AB | 2 (9.1%) | 2 (5.9%) | 0.97 | |
| Donor O | 7 (31.8%) | 11 (32.3%) | 0.97 | |
| ABO Seromatch | 11 (42.3%) | 19 (48.7%) | 0.61 | |
| Rhesus Seromatch | 18 (81.8%) | 23 (67.7%) | 0.24 | |
| WIT (mins) | 964.4±378.9 | 846.1±393.4 | 0.22 | |
| Conduit Diameter (mm) | 5.5±1.6 | 5.6±1.3 | 0.73 | |
a The reference group used was the femoral-popliteal bypass group.
Back to 2018 Abstracts




