Long Term Outcomes of Carotid-Subclavian Bypass in the Setting of Thoracic Endovascular Aortic Repair
Soraya L Voigt, Muath Bishawi, Richard L McCann, G. Chad Hughes, IV
Duke University, Durham, NC
BACKGROUND – Subclavian artery revascularization is frequently performed in the setting of thoracic endovascular aortic repair (TEVAR) for a variety of indications ranging from prophylactic prevention of upper extremity and spinal cord ischemia to preservation of hemodialysis access or left internal mammary artery coronary artery bypass graft. Despite this, there is little information on the short and long-term outcomes of patients undergoing carotid to subclavian artery bypass. We sought to define the outcomes associated with this procedure.
METHODS – Patients undergoing carotid-subclavian bypass in conjunction with TEVAR between 6/2005 and 9/2016 were retrospectively identified from a prospectively maintained, single-center aortic surgery database. Categorical and continuous variables were compared using chi-squared and Wilcoxon rank sum tests, respectively. 30-day outcomes specific to the carotid-subclavian bypass procedure were analyzed including nerve injury, bleeding complications, and local vascular complications. All pre- and postoperative chest x-rays were carefully analyzed to assess for hemi-diaphragm elevation indicative of phrenic nerve palsy. Long term outcomes included primary graft patency and anastomotic complications.
RESULTS – Of n=579 patients undergoing TEVAR during this time interval, 114 patients (20%) underwent concomitant carotid-subclavian bypass. The cohort was 39% female (n=44) with a mean age of 65±14. The vast majority of conduits were 8 mm PTFE grafts (n=107; 92.2%), with a minority being reversed saphenous vein grafts (n=4; 3.5%). The bypass procedure was done concomitantly at the time of TEVAR in 90.4% (n=103) of cases. The short-term complication rate attributed specifically to the carotid-subclavian bypass was 21% (n=24). These complications included neck hematoma requiring re-exploration 0.9% (n=1), recurrent laryngeal nerve palsy 5.3% (n=6), axillary nerve palsy 1.8% (n=2), and phrenic nerve palsy in 13.2% (n=15) of patients. The 30-day all-cause mortality rate was 5.3% (n=6), and the rate of permanent paraparesis/paraplegia was 0.9% (n=1). Of the operative survivors (n=108), follow up imaging of the bypass graft was available in 84% (n=96) of patients. Actuarial primary graft patency was 97% at 10 years (figure). There were three patients (2.5%) with bypass graft occlusions, two of which were clinically silent and detected in follow up imaging. The third was detected due to the symptoms of subclavian steal and required repeat revascularization. Two patients (1.8%) developed a late anastomotic pseudoaneurysm requiring either endovascular (n=1) or surgical (n=1) intervention.
CONCLUSIONS – Carotid-subclavian bypass for revascularization of the subclavian artery performed in the setting of TEVAR is durable, although the true complication rate is likely higher than generally reported in the literature due to a non-insignificant rate of phrenic nerve palsy. These data should serve well as gold-standard comparison data for emerging branch graft devices. 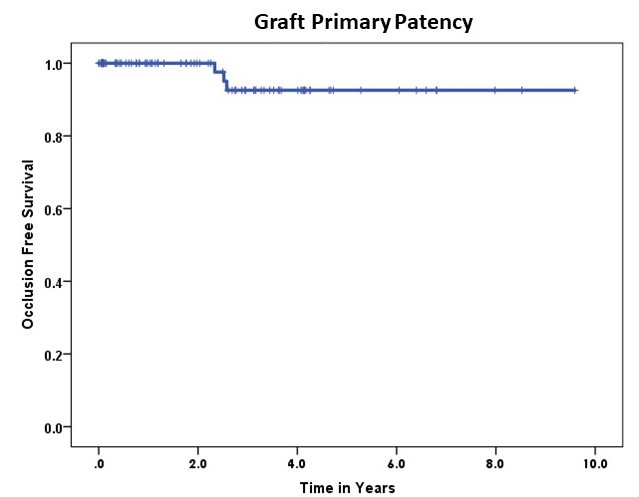
Back to 2018 Abstracts




