Aorto-iliac calcification correlates with 5-year survival following abdominal aorta aneurysm repair
Matthew TerBush, Khurram Rasheed, Zane Z Young, Jennifer L Ellis, Roan J Glocker, Adam J Doyle, Kathleen Raman, Michael C Stoner
University of Rochester, Rochester, NY
Introduction
In 2002, the Committee for Standardized Reporting Practices in Vascular Surgery of the Society for Vascular Surgery/American Association for Vascular Surgery proposed an anatomic severity grade (ASG) score to categorize and define anatomic factors as they relate to infrarenal abdominal aorta aneurysms (AAA) [1]. The original purpose of this score was to quantitatively assess anatomic complexity of the aorta prior to undertaking a repair. Our group previously reported that aortic anatomic complexity is a marker of atherosclerotic risk and resource utilization at the time of repair [2,3]. However, it remains unclear whether individual components to this score - specifically the aortic and iliac calcium burden - independently contributes to mid-term survival after AAA repair. The purpose of this study is to analyze and validate an aortic and iliac artery calcium scoring system that can predict mid-term mortality after AAA repair. These data have direct implications for the population management based treatment of aortic aneurysmal disease.
Methods
Patients with complete 5-year records who underwent open and endovascular infrarenal AAA repairs between July 2007 to May 2012 at the University of Rochester Medical Center were retrospectively identified using Current Procedural Terminology (American Medical Association, Chicago, Ill) codes 34800, 34802, 34803, 34804, and 34805. To avoid potential interference from perioperative mortality, those who expired within 30 days of surgery were not included. Degree of vessel calcification was obtained from preoperative CT scans no more than 6 months before surgery, calculated manually using three-dimensional reconstruction software (Philips Intellispace Portal; Koninklijke Phillips Electronic NV, Andover, MA) by two blinded reviewers. Calcium Score (CS) was defined using the ASG scoring system for its basis [1]. The scoring is as follows:
For aortic neck calcium:
• 0 points for less than 25% calcium
• 1 point for 25-50% calcium
• 2 points for 51% or greater calcium
For iliac calcium:
• 0 points for no calcium
• 1 point for less than 25% calcium
• 2 points for 25-50% calcium
• 3 points for 51% or greater calcium
A possible CS for any patient is between 0-5 points (the sum of the aortic and iliac calcium points). A receiver-operator curve (ROC) was developed to determine an appropriate CS threshold for analysis. Kaplan-Meier survival curves of the groups defined by this threshold were compared with log rank and Wilcoxon sign rank tests, with statistical significance of p<0.05.
Patients who survived and those who did not were compared in regards to the following variables: CS, sex, race, age at time of surgery (age), hypertension (HTN), hyperlipidemia (HLD), diabetes (DM), coronary artery disease (CAD), chronic obstructive pulmonary disease (COPD), chronic kidney disease (CKD), end stage renal disease (ESRD), presence of neoplasms (NEO), and specific pharmacologic therapies (beta blockers, ACE inhibitors, aspirin, Plavix, and statins). The Pearson χ2 test was used to compare categorical variables, and the Student t test was used to compare continuous variables between the two groups. Each variable with a p-value <0.1 between the groups was then placed into a Cox proportional hazards model, with statistical significance of p<0.05. All statistical analysis was performed using SAS software Version 9.4 (SAS Institute Inc.; Cary, NC).
Results
356 patients underwent AAA repair had complete calcium and survival data who did not expire within 30 days of AAA repair during our study period. 93/356 (26%) expired within 5 years of AAA repair. 47/356 (13%) had CS=0 with 7 (15%) mortalities, 98/356 (28%) had CS=1 with 21 (21%) mortalities, 86/356 (24%) had CS=2 with 21 (24%) mortalities, 83/356 (23%) had CS=3 with 29 (35%) mortalities, 35/356 (10%) had CS=4 with 14 (40%) mortalities, and 6/356 (2%) had CS=5 with 1 (17%) mortality.
The developed ROC from this data demonstrated an appropriate threshold of CS=3, with area under the curve of 0.61. 231/356 (65%) had a CS less than 3, while 125/356 (35%) had a CS 3 or greater. These two populations were similar, except those with CS 3 or greater had higher rates of COPD (31.2% vs 16%, p=0.0008) and female gender (25.6% vs 16%, p=0.0290). Figure demonstrates the 5 year Kaplan-Meier curves of these 2 groups, with a statistically significant greater 5 year mortality probability in patients with a CS 3 or greater (35.2% vs 21.2%, log rank p=0.0030 and Wilcoxon p=0.0032).
When comparing the 5 year mortality and survivor groups, CKD (15.1% vs 6.8%, p=0.0173), ESRD (3.2% vs 0%, p=0.0034), COPD (30.1% vs 18.2%, p=0.0164), beta blocker usage (87.1% vs 78.7%, p=0.0769), age (average of 77 vs 71, p<0.0001), and CS 3 or greater (47.3% vs 30.8%, p=0.0041) had p<0.1 and appropriate to be used for a Cox proportional hazards analysis. Table demonstrates the results of this analysis. CS of 3 or greater was associated with a statistically significant hazard ratio (HR) of 1.579 (95% CI 1.038-2.402, p=0.0328). ESRD (HR=9.013, 95% CI 2.925-27.776, p=0.0001) COPD (HR=1.804, 95% CI 1.138-2.860, p=0.0121), and age (HR=1.065, 95% CI 1.037-1.093, p=<0.0001) were also associated with HR>1.
Conclusions
The calcium scoring system presented herein is the first known system that validates a calcium scoring scheme that can signify increased mid-term mortality after AAA repair. The degree of vessel calcification has been known to signify an overall burden of vascular disease, which has been examined in other specialties, including cardiology, and linked to mortality. In 2015, Shaw et al published a cohort study which demonstrated a coronary calcification score accurately predicting 15 year all-cause mortality in 9715 asymptomatic patients. Those with no score experienced a 3% mortality rate, while in those with a score of 1000 or more experienced a 28% mortality rate [4]. Our system potentially can be another measure to risk stratify patients undergoing a AAA repair and serve as a means to predict mid-term mortality probability. This study serves as a stepping stone in using this validated scoring system as a guide in decision making in surgical intervention of AAAs at both the patient and population levels. These data have the potential to assist value-based decisions in a variety of vascular disease states.
Limitations to this study include that it was retrospective in nature, only covered a particular population of AAA patients, does not include non-repaired cases, lacked data points at the extremes of CS (less patients had a CS of 0 or 5), and that the means of calcium measurement were done manually, as automated software to do this does not yet exist. Future data will be needed to further validate this scoring system in predicting mid-term mortality in patients undergoing AAA repair and to further develop the system in guiding decision making in surgical repair of AAAs.
References
[1] Chaikof EL, Fillinger MF, Matsumura JS, Rutherford RB, White GH, Blankensteijn JD, Bernhard VM, Harris PL, Kent KC, May J, Veith FJ, Zarins CK. Identifying and grading factors that modify the outcome of endovascular aortic aneurysm repair. J Vasc Surg. 2002;35:1061-1066
[2] Young Z, Trakimas LE, Glocker RJ, Doyle AJ, Mix D, Ellis JL, Stoner MC. Aortic Anatomic Severity Grade Correlates With Midterm Survival in Patients Undergoing Aortic Aneurysm Repair. J Vasc Surg. 2016;63 Supplement:164S-165S
[3] Rasheed K, Cullen JP, Seaman MJ, Messing S, Ellis JL, Glocker RJ, Doyle AJ, Stoner MC. Aortic anatomic severity grade correlates with resource utilization. J Vasc Surg. 2016;63(3):569-576
[4] Shaw LJ, Giambrone AE, Blaha MJ, Knapper JT, Berman DS, Bellam N, Quyyumi A, Budoff MJ, Callister TQ, Min JK. Long-Term Prognosis After Coronary Artery Calcification Testing in Asymptomatic Patients: A Cohort Study. Ann Intern Med. 2015;163(1):14-21
Figure - Kaplan-Meier curves demonstrating the 5 year survival probabilities for patients with CS less than 3 and CS 3 or greater.
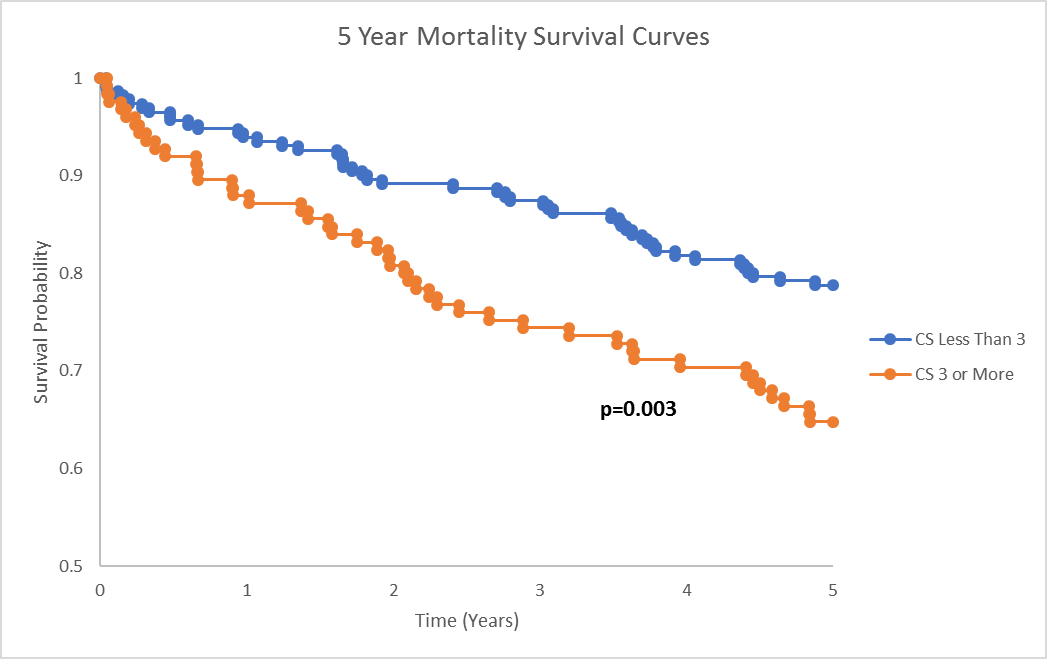
Table - Cox proportional hazards model results for factors with p<0.1 when compared to the patients who expired and those who survived within 5 years after AAA repair.
| Parameter | Hazard Ratio | 95% Confidence Limits | p-value |
| CKD | 1.408 | 0.751-2.637 | 0.2858 |
| ESRD | 9.013 | 2.925-27.776 | 0.0001 |
| COPD | 1.804 | 1.138-2.860 | 0.0121 |
| Age | 1.065 | 1.037-1.093 | <0.0001 |
| CS 3 or greater | 1.579 | 1.038-2.402 | 0.0328 |
| Beta blocker usage | 1.579 | 0.858-2.907 | 0.1421 |
Back to 2018 Abstracts




