Lower Extremity Neurological Impairment after FEVAR
Bernandino Rocha, Jonathan Braun, Joseph L Mills, Houssam Younes, Neal R Barshes, Panos Kougias
Baylor College of Medicine, Houston, TX
Lower Extremity Neurological Impairment after FEVAR
Background: Placement of large transfemoral sheaths through the iliac system during fenestrated endovascular aneurysm repair (FEVAR) leads to lower extremity (LE) ischemia that is associated with serious neurologic complications. We sought to determine the effect of the continuous lower extremity ischemic time (cLEIT) on neurological impairment after FEVAR.
Methods: Consecutive patients who underwent FEVAR at a single institution were analyzed. cLEIT was calculated from the time of large sheath (at least 18 Fr) insertion to the time of sheath removal from the iliac arteries that led to continuous LE ischemia. Common iliac artery (CIA) lumen was defined as diameter of the truly patent lumen of a CIA. Neurological impairment was defined as any new sensory or motor deficit in either LE. Outcomes were summarized with descriptive statistics and modeled with logistic regression with interaction terms. Individual lower extremity was used as the unit of analysis
Results. We examined 101 patients (202 extremities) who underwent FEVAR over a 5-year period. The median cLEIT was 2.75 hours (Range: 1.3 - 5.2 hours). Neurological impairment developed in 18 (9%) of the extremities. Among those 18 affected extremities 12(67%) developed mild sensory loss, 8(13%) complete sensory loss, 4(22%) loss of proprioception, and 2(11%) motor dysfunction. Sensory deficit was permanent in 4(2%) and motor dysfunction in 1(0.5%) of the total extremities assessed. In all other cases neurologic status returned to normal by postoperative day 15 (median recovery: 4 days, range 1 to 14 days). One patient (both LEs) underwent fasciotomy postoperatively. There were no amputations. Duration of cLEIT (OR: 21.6, 95% CI: 8 to 57.6, p< 0.001) and CIA lumen 8mm or less (OR: 5.7, 95% CI: 1.8 to 17.8, p=0.002) were independent predictors for the development of neurological impairment. An interaction term between cLEIT and CIA lumen 8mm or less was significant statistically (p=0.042) indicating that the presence of small CIA lumen modifies the effect of cLEIT. As shown in Figure 1, in patients with CIA lumen 8mm or less, the risk of neurological impairment increases rapidly after 2.5 hours of LE ischemia, and becomes nearly certain after 4 hours of ischemic time. In contrast, patients with larger CIA can tolerate a longer duration of ischemia and demonstrate a less steep rise in the risk for LE neurological impairment.
Conclusions: Lower extremity neurological impairment after FEVAR is strongly associated with cLEIT and patent CIA lumen 8mm or less. Our data indicates that when the LE continuous ischemic time is expected to exceed 2.5 hours (in patients with small CIA) or 3 hours (in patients with CIA lumen greater than 8mm), measures to assure perfusion of LEs during should be undertaken.
Figure 1 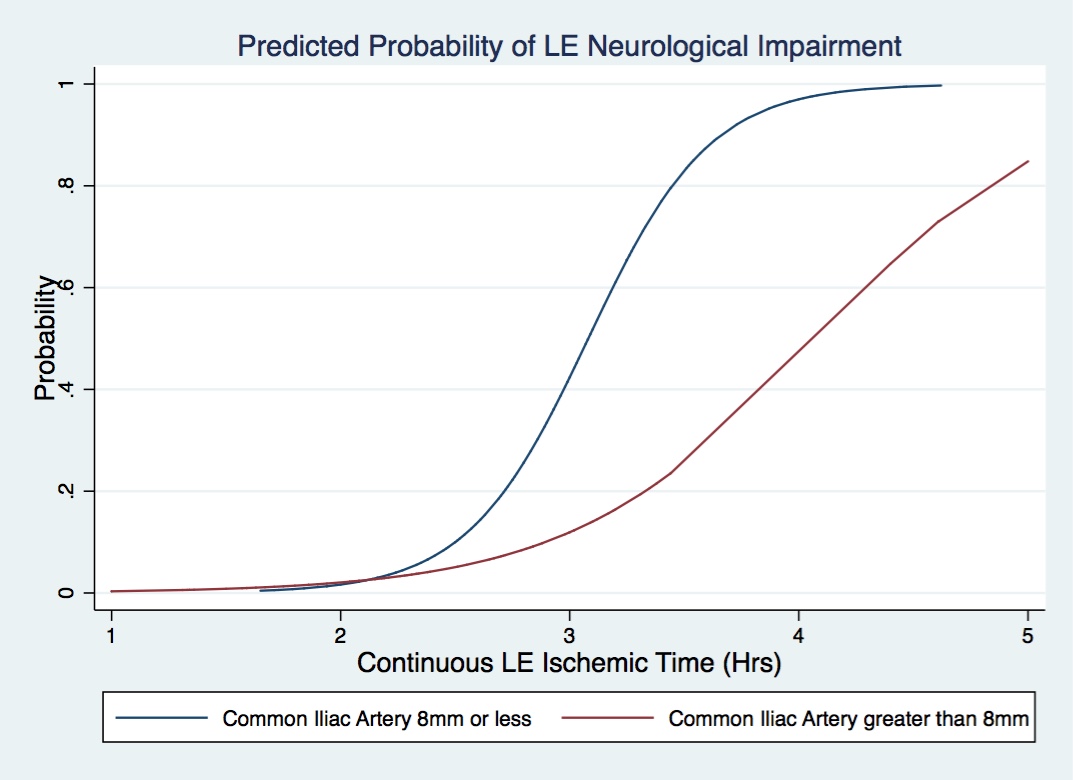
Back to 2018 Abstracts




