Renal Volumes and eGFR Changes After Fenestrated-Branched Aortic Repair
Fernando Motta, Corey A. Kalbaugh, Jason Crowner, Jason P Fine, Daniel J Luckett, Ioana Antonescu, Elad Ohana, Mark A Farber
University of North Carolina, Chapel Hill, NC
Background: Describe changes in renal volumes and renal function after Fenestrated-Branched Endovascular Repair(F-BEVAR) for complex aortic aneurysms.
Methods: Between July 2012 and April 2017, patients enrolled in a Physician Sponsored Investigational Device Exemption(PSIDE) clinical trial for the endovascular treatment of complex aortic aneurysms had data analyzed retrospectively. The prospectively maintained database included pre-operative demographics, comorbidities, preoperative computed tomography angiography(CTA) results, duplex ultrasound findings, perioperative data, and follow-up outcomes. Descriptive statistics were calculated using mean and standard deviations. Mean estimated glomerular filtration (eGFR) and renal volumes were calculated for baseline and each time point (6, 12, and 18 months post-procedure). A linear model was used with generalized estimating equations (GEEs) to determine renal volume predictive modeling of eGFR and adjusted for patient characteristics and co-morbidities. The analysis was also adjusted for patient’s preoperative renal status and the presence of accessory renal arteries.
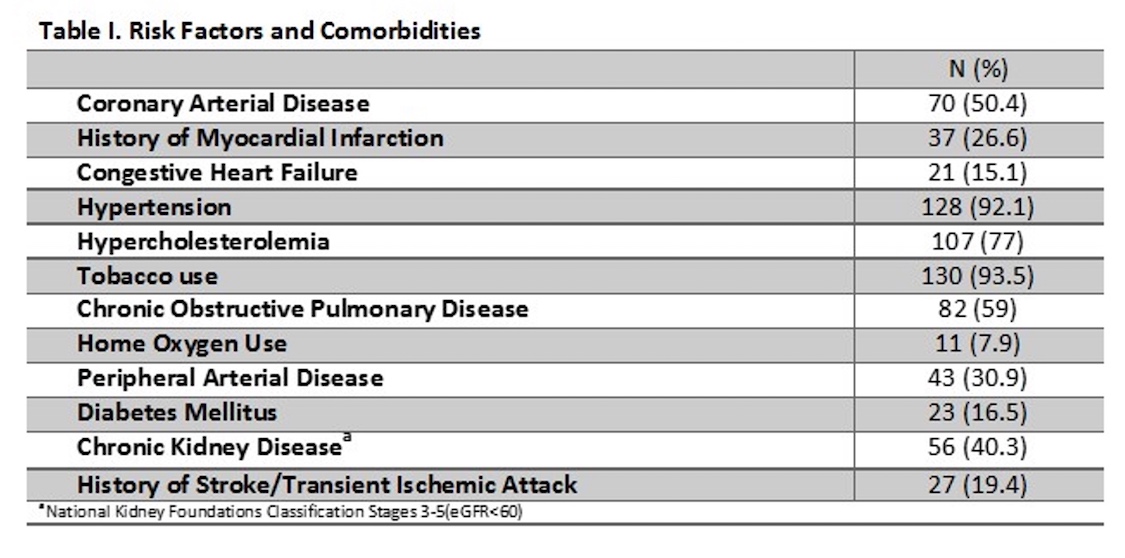
Results: Over the study period, 139 patients were included for analysis and followed for 18 months or until death. The mean age was 71+ 8 years; 70% of which were male. The most common risk factors were smoking history (94%) and hypertension (92%; Table I). Chronic kidney disease (eGFR<60 ml/min) was present in 40% (56/139). Thirty-one patients (22%) had at least one accessory renal artery, 87% (27/31) of which were embolized or covered. On average, eGFR changed over time with a mean decrease of 4.6(±15.2) ml/min, 3.8(±15.4) ml/min and 5.0(±15.9) ml/min compared to baseline at the 6, 12 an18 month follow-up time intervals respectively. Similarly, renal volumes decreased from baseline: 8% (±17), 10% (±17) and 11% (±22) at 6, 12 and 18 months, respectively. An increase in the patient age of 5 years was estimated to be associated with a decrease of 2.9 ml/min in eGFR, which is similar to the natural history of renal deterioration with age. There was an estimated decrease of 1 cm3 in renal volume for each decrease of 0.05 ml/min in eGFR(p=0.047). The average change in renal volumes among patients with and without previous CKD was not statistically different. Interestingly, 16.1%(9/56) of patients with previous CKD had improvement in their eGFR to >60 ml/min, all of which were stage 3. The mean follow-up for the cohort was 14.3 months. Kaplan-Meier survival at 1 and 2 years was 84.7% and 78.8%.
Conclusion: Renal volume and eGFR decreased in patient undergoing repair at similar rates to natural history progression. The eGFR was found to moderately correlate with renal volume. Most accessory renal arteries can be excluded without significant impact on renal function. The majority of the decline in renal function occurred within the first six months post-operatively, after which stabilization was observed suggesting little impact of F/BEVAR on renal function during the initial 18 months after treatment.
Back to 2018 Abstracts




