Case Report: Aortic Agenesis and Renal Transplantation using the Hepatic Artery as Inflow
James M Chang, Danielle J Haakinson, Victor J Davila, Kunam S Reddy, Adyr A Moss, Samuel R Money
Mayo Clinic Arizona, Phoenix, AZ
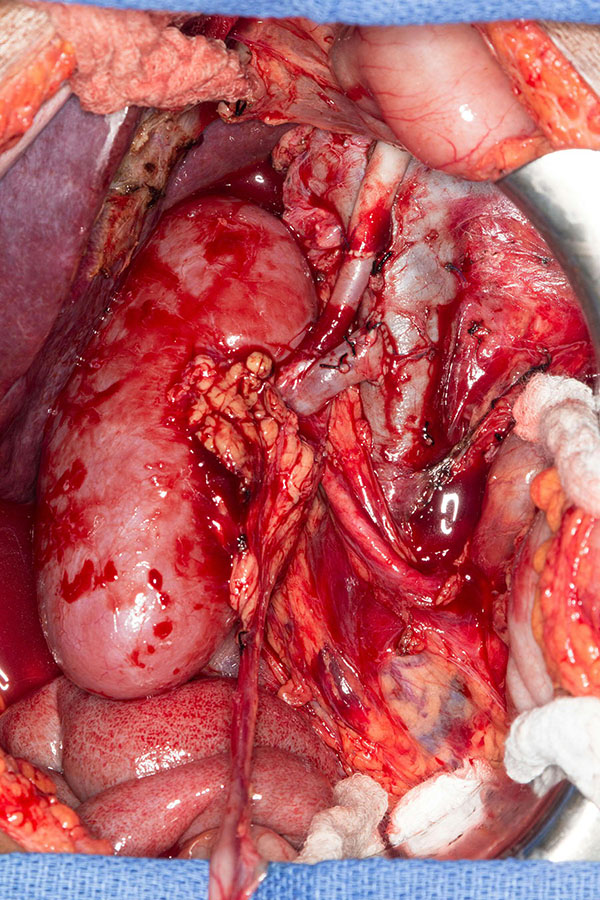
INTRODUCTION: Aortic atresia is a rare condition with congenitally absent or diminutive abdominal aorta, associated with renal failure and presenting unique challenges to renal transplantation with regard to arterial inflow for the allograft. METHODS: This is a case report. RESULTS: A 25 year-old female presented with a history of renal failure secondary to aortic agenesis to transplant clinic. She had previously been denied transplant at other institutions given her unique vascular anatomy. As an infant, the patient had hypertension and renal failure necessitating peritoneal dialysis. Initially she was thought to have coarctation of the aorta, however subsequently was noted to have aortic agenesis below the level of the celiac artery, both native kidneys were hypoplastic supplied by paraspinal collateral arteries. Peritoneal dialysis was discontinued a few weeks after birth and the patientís renal function largely recovered until she began hemodialysis 3 years prior to evaluation. Computed tomography angiography demonstrated aortic agenesis below the level of the superior mesenteric artery. Lower extremities were supplied by abdominal wall collaterals. After evaluation of her by the transplant selection committee, she was approved for transplant. Preoperative evaluation was conducted with the vascular surgery service as well given her unique anatomy. A deceased donor kidney with standard arterial, venous, and ureteral anatomy was offered to the patient and accepted. The aortic arch of the donor was also harvested for use as conduit. A midline laparotomy was made and the inferior vena cava and the common hepatic artery were dissected and isolated. The donor left common carotid was used as a jump graft from the common hepatic artery to the donor renal artery. Donor renal vein was anastomosed to the inferior vena cava. A right native nephrectomy was performed and the donor allograft was placed in the right retroperitoneum. Standard extravesical ureteroneocystostomy over a stent was performed. The patient was hospitalized for four days post-operatively without any further dialysis. One year post-transplant evaluation demonstrated a normal creatinine of 1.0 mg/dl. CONCLUSIONS: The hepatic artery as use for inflow in renal transplantation has been rarely reported and not previously using donor vessels as conduit. This technique was successful in this unique patient and may be a viable approach for other patients with variant anatomy. 
Back to 2018 Abstracts




