Risk of Multiple Versus Single Stent Use in Carotid Stenting Outcomes
Muhammad Faateh, Muhammad Rizwan, Besma Nejim, Satinderjit Locham, Hanaa Dakour Aridi, Mahmoud B Malas
Johns Hopkins Medical Institutions, Baltimore, MD
INTRODUCTION: Results from large randomized controlled trials including CREST have suggested lesion length to be an important predictor of adverse outcomes following carotid artery stenting (CAS). Longer lesions require multiple stents, however, the associated risks following multiple stents remain largely unknown. Therefore, the purpose of this study is to determine adverse outcomes following single versus multiple stents in patients undergoing CAS.
METHODS: All patients in Vascular Quality Initiative (VQI) Database from 2005-2017 undergoing CAS for Internal carotid artery and bifurcation lesions were included in the study. Any patients with more than two stents were excluded . Patients were then divided into two groups, those receiving single stents and those receiving two stents. Baseline demographics and characteristics were compared using ttest, chi-square or fisher’s exact test as appropriate. Univariate and multivariate regression analysis were used to compare In-hospital outcomes. All models were tested using Receiver operating curves.
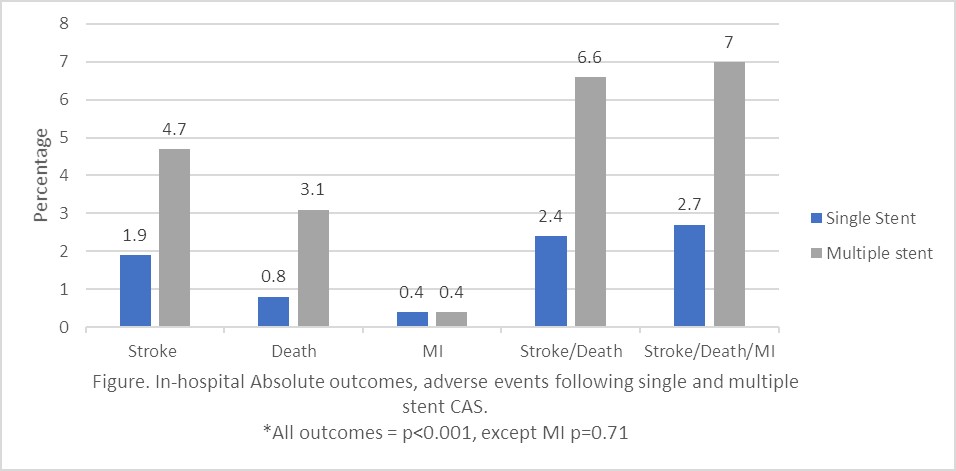
RESULTS: A total of 10,901 patients underwent CAS {Single stent: 10,385 (95%) and Multiple stent: 516(5%)}. Patients undergoing multiple stents were relatively younger [(mean age +-S.D.): 66.7(12.9) vs 69.6(10.2), p<0.001] and less likely to be hypertensive (84.7% vs. 89.4%, p<0.001) compared to patients with single stent. All other comorbidities were similar between the two groups. Patients receiving multiple stents were more likely to have occlusive lesions (11.3% vs. 3.4%) and were more likely to undergo general anesthesia (25.6% vs 14.4%) (both p<0.001). Post-stent dilation was more frequent following single versus multiple stents (77.9% vs. 71.5%, p<0.001). In-hospital adverse outcomes including stroke (4.7% vs 1.9%, p<0.001) and death 3.1% vs 0.8% (p<0.001) were significantly higher in patients undergoing multiple stents compared to single stent (see figure). After adjusting for patient demographic, comorbidities, symptomatic status, anesthesia types, ballooning time, and perioperative medications, multivariate logistic regression analysis showed a 2-3-fold increase risk of stroke (OR 2.96, 95%CI 1.81-4.87, p<0.001) and death (OR 2.33, 95%CI 1.13-4.81, p=0.02) in patie nts with multiple stents compared to single stents (Table).
CONCLUSIONS: Using a large national multicenter database, we demonstrate that patients undergoing multiple stents had a three-fold increase risk of stroke and greater than two-fold increase risk of death compared to patients with single stents. As multiple stents are in essence a surrogate marker of lesion length, a greater proportion of these risks may be attributed to lesion length. Carotid endarterectomy might be a better option for patients with longer and more extensive lesions.
| Univariate logistic regression, Multiple vs single stents. Odds Ratio (95% CI) | P-Value | Multivariate* Logistic regression, Multiple stents vs single stents, Odds ratio (95% CI) | P-Value | |
| Stroke | 2.59(1.68-3.99) | <0.001 | 2.96(1.81-4.87) | <0.001 |
| Death | 3.83(2.23-6.58) | <0.001 | 2.33(1.13-4.81) | <0.02 |
| MI | 1.07(0.26-4.43) | 0.93 | 0.64(0.09-4.83) | 0.67 |
| Stroke/Death | 2.83(1.96-4.09) | <0.001 | 2.57(1.63-4.01) | <0.001 |
| Stroke/Death/MI | 2.72(1.90-3.90) | <0.001 | 2.41 (1.54-3.75) | <0.001 |
Back to 2018 Posters




