The Implementation of a Vascular Preventative Bundle to Decrease Surgical Site Infections: Early Institutional Experience
Ehsan Benrashid, Kimberly Guest, Christopher R Mantyh, Cynthia K Shortell, Ellen D Dillavou
Duke University, Durham, NC
Background: Surgical site infection (SSI) rates correlate with readmissions, reoperations, increased length of stay, and amputations. Benchmarking data through the National Surgery Quality Improvement Program (NSQIP) provides a means for institutions to assess their own infection rates. The current study describes our multidisciplinary institutional approach using vascular surgery-targeted variable bundle modification of pre, peri-, intra- and post-op care for SSI reduction in groin and leg wounds.
Methods: Vascular surgery patients with groin and/or lower extremity incisions from October 2015 through July 2017 were identified from the medical record. Pre-operative optimization included glucose control and anemia. Perioperative optimization included directed hair clipping, use of chlorhexidine gluconate (CHG) wipes, and revised systems for antibiotic administration. Intra-op improvements included: decreasing room traffic, tighter glucose, temperature and anemia control, use of dedicated closure trays, standardization of wound closure methods and variable use of a surface negative pressure wound therapy (NPWT) closure system. Post-operative improvements included standardization of wound care. Changes were enacted over a 6 month period, with representatives from vascular surgery, nursing, infectious diseases, anesthesia, pharmacy, hospital administration, and electronic medical records involved.
Results: Prior to the reduction effort, SSI rate was 7.44% in October 2015, decreasing to 3.01% in April 2017 according to NSQIP data. Bundle implementation was from November 2015 to June 2016, and NPWT was initiated April 2016. Rate of pre-op hair clipping went from 73.3% in January 2016 to 77.9% in July 2017; use of CHG wipes 50.6% and 86%; and use of the closure tray was 39% and 87.5% in the same period. All patients received antibiotics and 92.1% received optimal dose and timing in July 2017, compared to 52.2% in April of 2016. 318 patients had groin and/or lower extremity incisions during the study period. 157 had NPWT, 161 had standard dressings. Total readmissions were 26.1% and 41.6% for NPWT and standard groups, respectively (p = 0.002). Readmissions for infection were 9.6% (NPWT) and 14.9% (standard) (p = 0.15). 7.6% (NPWT) and 13.0% (standard) had return to OR (RTOR) for infection (p = 0.11). 3.14% of patients (n =10) had postoperative seromas mandating RTOR, 0.64 vs. 5.59%, with and without NPWT (p = 0.01). Overall, patients receiving vascular procedures at our institution have had decreased rates of seroma requiring RTOR in 2017 than 2016, at 2.72% vs. 3.37%, respectively. As demonstrated in the Figure, implementation of the institutional vascular bundle has shown an overall trend toward decreased rates of postoperative SSI.
Conclusions: Multidisciplinary cooperation to create and use evidence-based practice bundles, coupled with perioperative staff education and compliance monitoring has yielded a decrease in institution-specific SSI. Negative pressure wound therapy may decrease seroma formation and possibly infection. 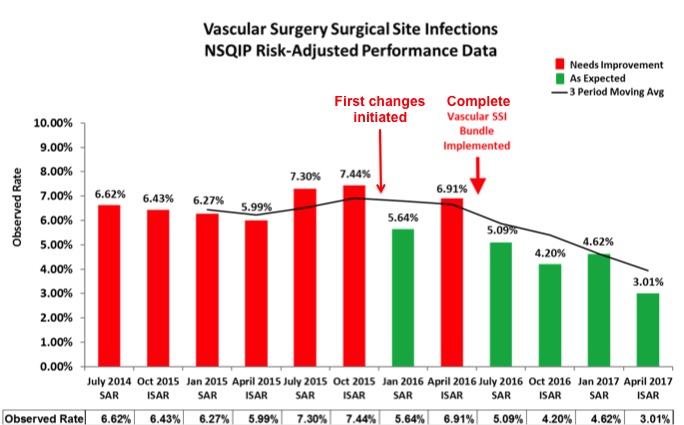
Back to 2018 Posters




