Current Attitudes and Practice of General Surgery Resident Experience in Vascular Surgery
Danielle C Sutzko1, Elizabeth A Andraska2, Matthew A Corriere1, Nicholas H Osborne1, Peter K Henke1
1University of Michigan, Ann Arbor, MI;2University of Pittsburgh Medical Center, Pittsburgh, MI
Background: Since the adoption of the integrated vascular training paradigm, there has been remarkable growth in the available training programs. Although there have been studies evaluating the GS (GS) case volume of vascular surgery residents, little is known on the impact 0+5 training programs have on GS resident experiences. While some have suggested little impact on GS case volume with the addition of integrated programs, a more targeted evaluation of vascular surgery programs is warranted.
Methods: An anonymous, 19-question survey was sent to all vascular surgery program directors across the United States (N=114). Participants were polled through Qualtrics from May 2017 to June 2017. The surveys consisted of multiple choice and free response questions. Analysis was completed using descriptive statistics.
Results: A total of 57 participants completed the survey (response rate 50%). The majority of program directors surveyed had fellowships with 1 position (56%, N=31) and no integrated vascular program (46%, N=26). All participants had GS residents with the most frequent number of residents being 6 per year (34%, N=19). The majority of participants reported the presence of integrated cardiac surgery residency programs (74 %, N=42). GS residents commonly rotated on vascular during the PGY-1 or -2 years (89%, N=50; 75%, N=42) and only 10 participants reported chief resident rotations (18%). The majority of GS residents had a total of 3-4 months on vascular surgery. The overall perception of GS residents rotating on vascular was that the amount was just right (52%, N=29), where 23 participants (41%) felt that too little time was spent on vascular surgery. Peripheral and
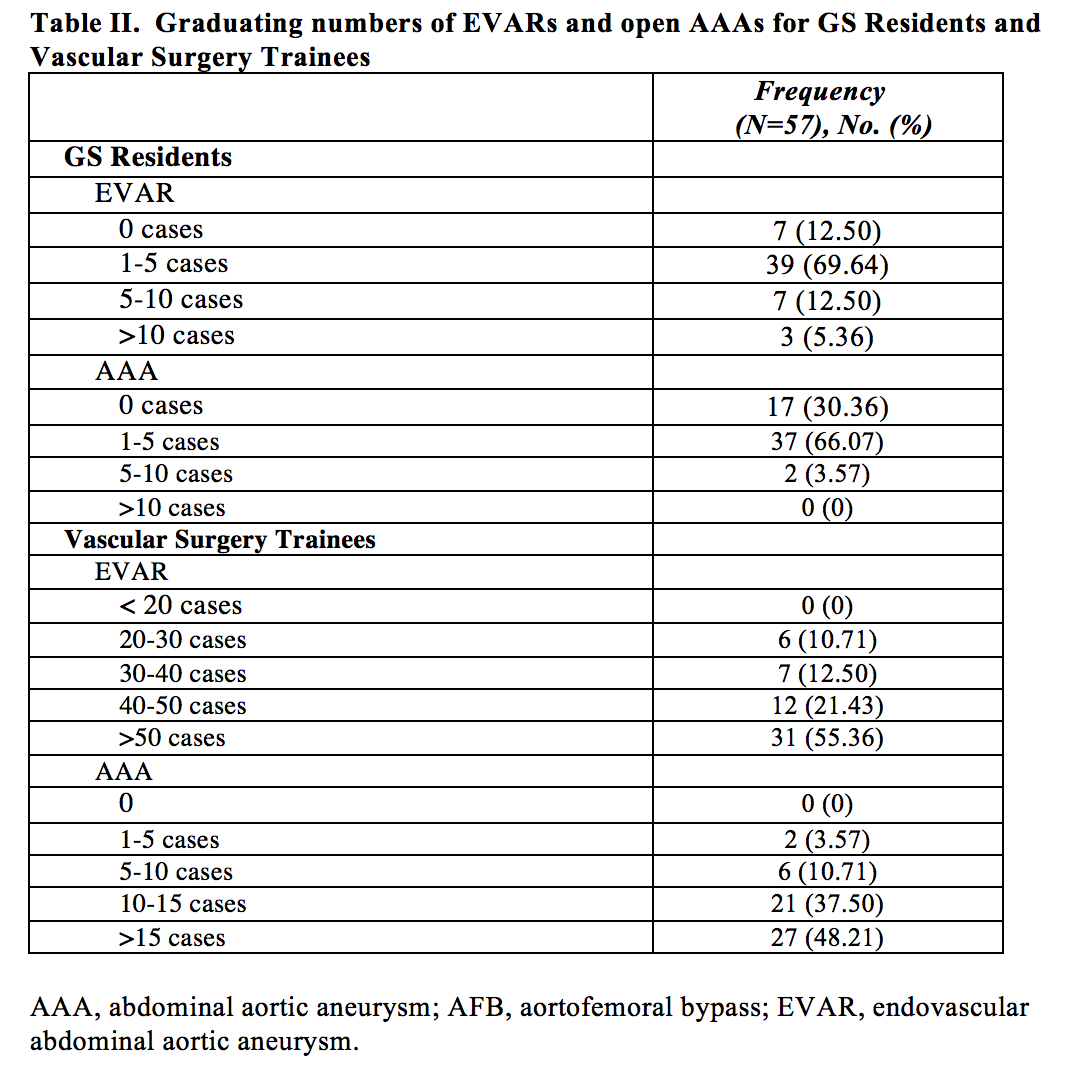
cerebrovascular operations were the most common procedures GS residents were exposed. Table I summarizes the exposure and appropriateness of Vascular Surgery operations when program directors were polled. GS residents were least likely to gain exposure to EVAR and complex vascular operations, which were in alignment with only 58% and 45.45% of participants considering these cases to be level appropriate. Although 75% of participants believed that the EVAR volume was adequate for GS residents, 70% responded that the GS residents graduated with only 1-5 EVARs. In contrast, 55% of participants responded that the vascular trainees performed >50 EVARs by graduation.
Conclusions:
Among responding vascular surgery programs, GS and integrated cardiac residents continue to rotate on vascular surgery; however, the majority do not as chief residents. The most common procedures performed are cerebrovascular and peripheral vascular. There is significant variation in perceptions of what procedures are considered appropriate for GS residents. As surgical training continues to evolve, the expectations of general surgeons experience in vascular surgery needs to be further defined. 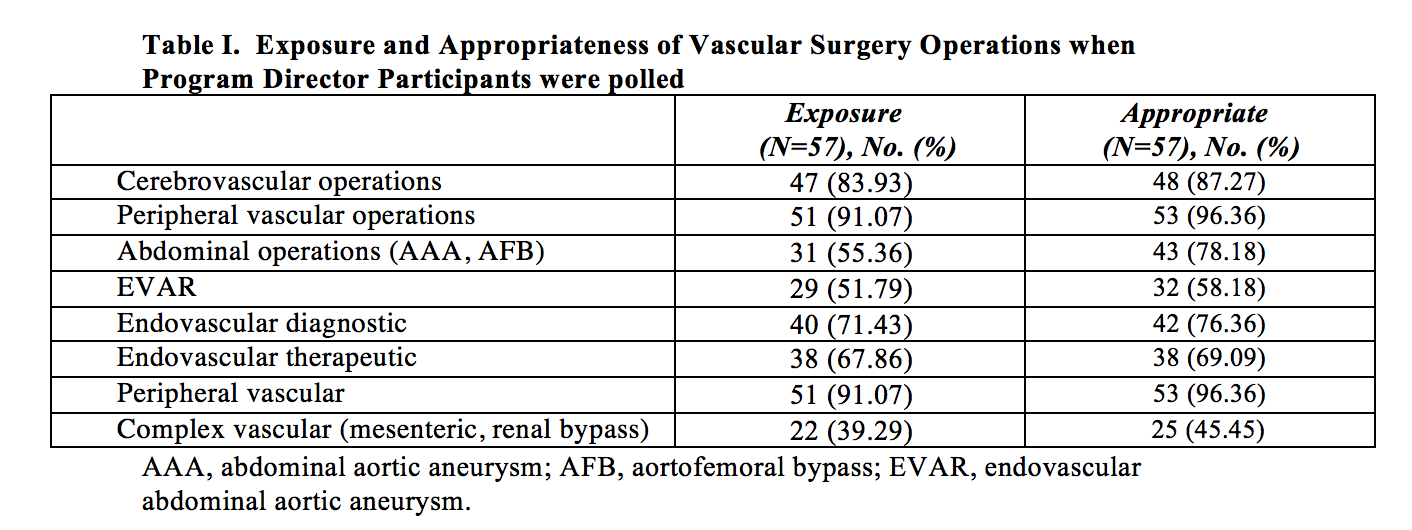
Back to 2018 Posters




