TYPE B AORTIC INTRAMURAL HEMATOMA: TO TEVAR OR NOT TO TEVAR?
Tomaz Mesar, Maggie J Lin, Ishraq Kabir, David Dexter, Animesh Rathore, Gordon K Stokes, Jean M Panneton
Eastern Virginina Medical School, Norfolk, VA
OBJECTIVE
Intramural hematoma (IMH) is on the spectrum of acute aortic syndrome but optimal management is poorly understood. The aim of this study was to evaluate outcomes of patients with type B intramural hematoma (IMH) after best medical therapy (BMT), and assess what variables are associated with failure of BMT
METHODS
A retrospective review from 2008 to 2018 was conducted on patients admitted for type B IMH. Patients were grouped into those who received emergent/urgent TEVAR on initial evaluation (Group 1) and those who received initial BMT (Groups 2-4). Group 2 received TEVAR during the index admission for failed BMT. Group 3 received endovascular treatment after discharge from initial hospitalization. Group 4 only received BMT.
RESULTS
There were 90 IMH patients identified; 25 patients received emergent/urgent TEVAR (group 1), 65 were managed initially with BMT (groups 2-4). Thirty patients received TEVAR during the index hospitalization for failed BMT at a mean of 5.2 days from admission (range 2-12 days) (group 2) for continuous pain and hypertension (12), worsening IMH (11), presence of PAU (6) and aneurysm (1). Fifteen patients were intervened on at a mean of 217 days from admission (range 12-1449 days) (group 3) with EVAR for aortic rupture and formation of a new PAU (2); TEVAR for new thoracic PAU (1), aneurysmal degeneration (10) and worsening IMH (2). Twenty patients were treated with BMT (Group 4), 6 had aneurysmal degeneration; 1 had worsening of PAU on repeat imaging but was lost to follow-up. The mean follow-up in Groups 1 – 3 was 31 months and 23 months in Group 4.
Post-operative 30-day mortality was 4/70 (5.7%); none were aortic-related. One delayed aortic-related death (1.5%) occurred 4 months after repair due to thoracic aortic rupture. Other complications: spinal cord ischemia in 2.8%, major stroke 2.8%. There were 12 aortic specific re-interventions in 7 of 68 patients (12%): redo-TEVAR (9), mesenteric angioplasty (1) and left subclavian artery embolization (1) and one hybrid repair after two previous TEVARs. Early reintervention rate was 5%.
Endpoints included aortic-related events and mortality: rupture, major stroke, spinal cord ischemia, progression to dissection or aneurysm, need for TEVAR or re-intervention. In Group 1 follow-up, aortic related events/mortality occurred in 7/25 patients: redo-TEVAR (3), spinal cord ischemia (1), post-operative aortic rupture (1), progression to dissection (1) and stent-graft induced new entry (1). All patients in Groups 2 and 3 failed BMT and required intervention for aortic related events. Group 4 had 7/20 patients with aortic related events. Freedom from aortic-related events and mortality at 36 months was significantly higher in Group 1 compared to Groups 2-4 (72% vs. 17.7%; p=0.001). Only IMH thickness predicted failure of BMT (p=0.05).
CONCLUSION
Best Medical Therapy for type B IMH is associated with a high failure rate and need for further interventions. TEVAR is a safe and effective treatment. IMH thickness predicts the failure of BMT. 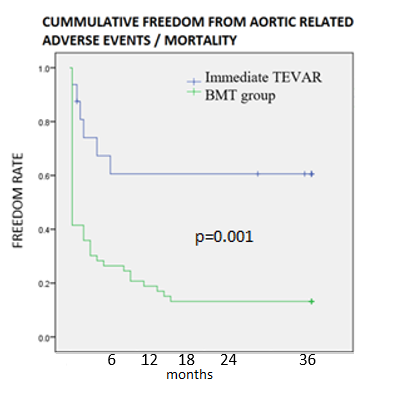
Back to 2019 Abstracts
