National Incidence, Mortality Outcomes, and Predictors of Spinal Cord Ischemia after Thoracic Endovascular Aortic Repair
Salvatore T. Scali1, Kristina A. Giles1, Grace J. Wang2, Thomas S. Huber1, Gilbert R. Upchurch1, Jeffrey J. Siracuse3, William P. Shutze1, Adam W. Beck4
1University of Florida- Gainesville, Gainesville, FL;2University of Pennsylvania, Philadelphia, PA;3Boston University Medical Center, Boston, MA;4University of Alabama at Birmingham, Birmingham, AL
INTRODUCTION: Spinal cord ischemia (SCI) is a dreaded complication of thoracic endovascular aortic repair (TEVAR). There are limited national data describing the incidence and influence of in-hospital SCI recovery on long-term survival. Moreover, no robust preoperative SCI risk assessment tools currently exist. The purpose of this analysis was to analyze the Vascular Quality Initiative (VQI) to determine the survival impact of SCI with or without in-hospital recovery, and develop a preoperative SCI prediction tool for patients undergoing TEVAR.
METHODS: All VQI TEVAR procedures (2011-18) were reviewed. The primary end-point was development of in-hospital SCI, defined as any new neurologic deficit and/or paralysis not attributable to intracranial pathology. Secondary end-points were disease-specific SCI rates and long-term out of hospital survival (verified through SSDI). Functional outcomes (transient vs. permanent SCI) were independently determined by treating physicians. Kaplan-Meier methodology was used to estimate survival. A logistic regression model of all candidate preoperative SCI predictors (P<.2) was created and backward step-wise elimination (in more than 50% of models) was used for model reduction. The model was validated by bootstrapping.
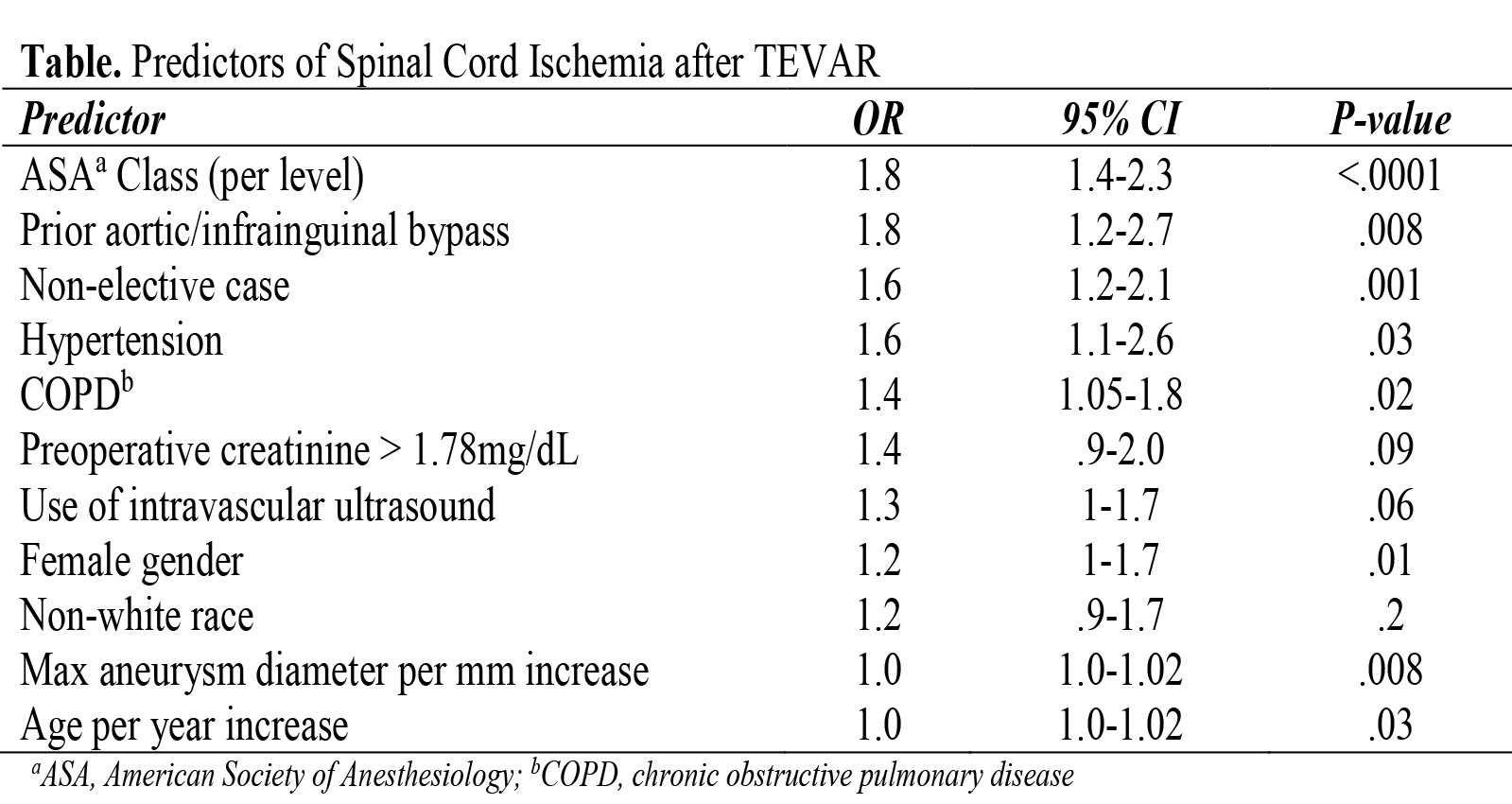
RESULTS: The overall rate of SCI was 4.7% (N=436 of 9217 patients; transient, 1.6% [n=148]; permanent, 3.1% [n=288]). The survival impact of SCI after TEVAR is highlighted in the Figure. Patients who developed SCI but had resolution of symptoms before discharge had similar survival to those without SCI (1-year: SCI with recovery 80±3% vs. No SCI, 89±1%; log-rank P-value = .06). However, patients without SCI in-hospital recovery had significantly worse overall survival (1-year: SCI without recovery, 62±3% vs. No SCI, 89±1%; P <.0001). Pathologic specific incidence of any SCI was: acute dissection (6.6%), intra-mural hematoma (6.4%), traumatic transection (5%), chronic dissection (4.6%), aortic thrombus (4.5%), degenerative aneurysm (4.2%), and PAU/IMH (3.2%). Several patient and procedure related factors were selected as the most important independent preoperative predictors of SCI (Table) (AUC = .75). This model had mean AUC = .71 with good model calibration (Hosmer-Lemeshow P=.7, Intercept=-.3, Slope=-.9).
CONCLUSIONS: SCI is a devastating complication after TEVAR that has a significant impact on overall survival, particularly when no functional recovery occurs by time of hospital discharge. Disease specific, real world benchmarks for SCI rates are provided which may inform quality improvement initiatives focused on reducing this complication. Importantly, this analysis is the first description of a preoperative prediction tool derived from national data for determining SCI risk after TEVAR. We have identified variables that can inform the use of interventions to mitigate SCI risk, thereby improving resource utilization and TEVAR outcomes nationally. 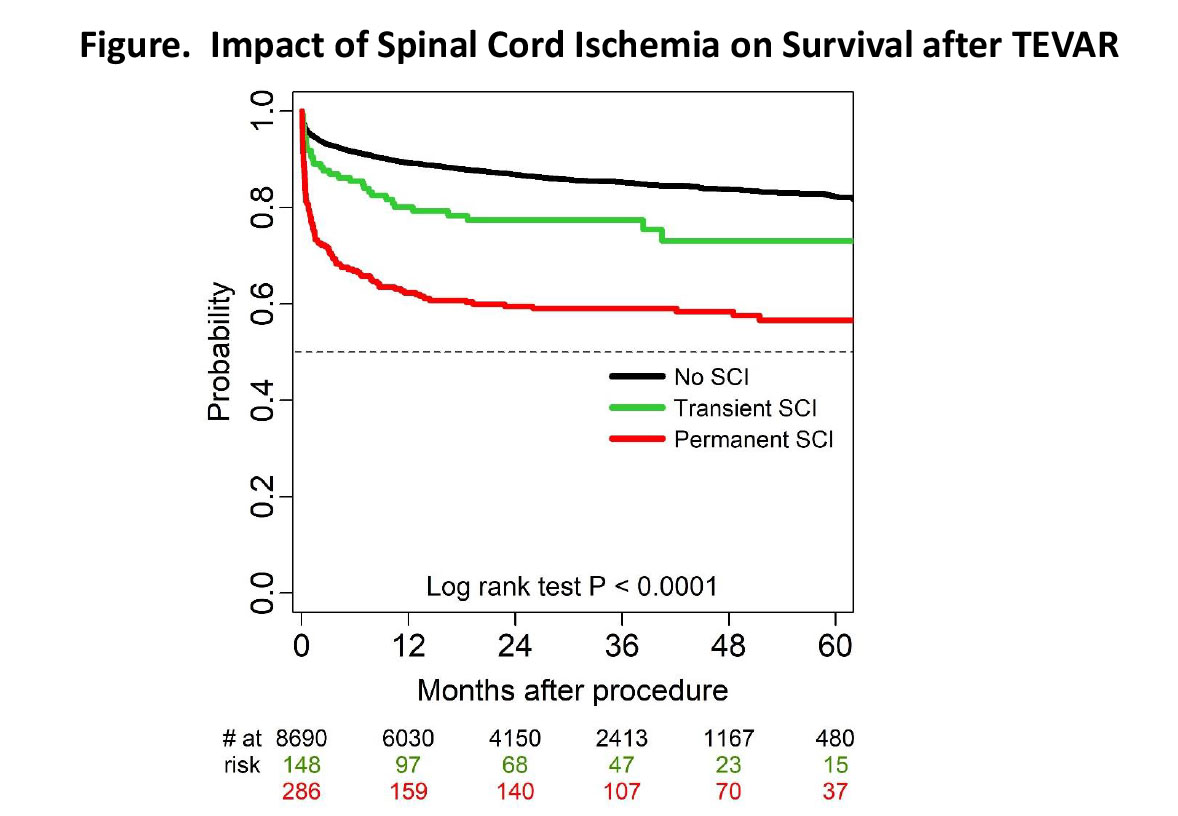
Back to 2019 Abstracts
