A Diagnosis and Treatment of Middle Aortic Syndrome
Lauren Story-Hefta, Mohammed Moursi
UAMS and Arkansas Children's Hospital, Little Rock, AR
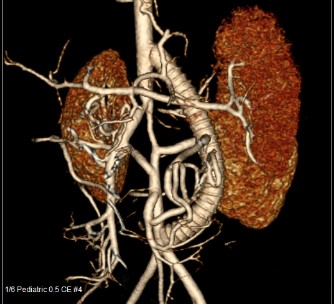
Middle aortic syndrome (MAS) is a disease manifested by segmental narrowing of the abdominal aorta and stenosis in the renal (70%) and visceral (33%) arteries. A 2.5-year-old, 13 Kg, female presented on 5/30/16 with flu-like symptoms. She was normotensive with femoral pulses. ECHO showed dilated cardiomyopathy with severe LV dysfunction. Oral heart failure therapy was started. Nine months later (Feb 2017) she returned decompensated with renal and liver failure and listed as status 1B for heart transplant. A Berlin L-VAD was placed in March 2017 and status was changed to 1A. The L-VAD improved heart function and uncovered hypertension and an upper/lower extremity pressure gradient. Cardiac cath revealed severe stenosis of the mid aortic segment with celiac occlusion, SMA stenosis and severe, bilateral renal artery stenosis. Aorta returned to normal caliber at the IMA with a 50mmHg gradient.On 3/15/17, she underwent open repair after pump change to CentriMag device. Subcostal incision was used and the viscera were rotated to the right. A supraceliac clamp was placed to allow for a bypass from supraceliac aorta to aortic bifurcation using an 8 mm ringed PTFE with 7-0 prolene in end-to-side fashion. Clamp time was 10 minutes. The left renal artery was transposed distally, to a normal caliber aortic segment, using 8-0 prolene. A 2.5 cm segment of the right internal iliac artery was harvested and used as an interposition bypass for the right renal artery, using an 8-0 prolene, with end-to-side anastomosis proximally and end-to-end anastomosis distally. The Berlin pump was replaced. Post-operatively, distal pulses were palpable and urine output was adequate. On POD 1, heparin was started due to clots in the L-VAD. Her abdomen became distended and hematocrit dropped. L-VAD was temporarily stopped, ECHO showed good ventricular function. She underwent washout and L-VAD removal. Post-operative course was benign, extubated on POD 11, weaned off pressors by POD 13, removed from transplant list and tolerating a regular diet by POD 16. Oral heart failure medications were restarted and resolution of end-organ failure was noted before discharge on POD 47. Post-operative renal duplex and CTA showed no stenosis of aortic graft, with mild stenosis of bilateral renal arteries. This is a unique presentation of MAS. She presented with dilated cardiomyopathy with no pressure gradient in upper and lower extremities. Once L-VAD was placed, cardiac output improved, but an upper/lower extremity pressure gradient developed. MAS was diagnosed. Her acute decompensation, requiring placement on transplant list, made operative repair to bypass her aortic stenosis and decompress her failing heart a viable option. The max assist L-VAD was removed, along with her name on the transplant list. She is now a 3-year-old girl running into the vascular lab for follow up studies. 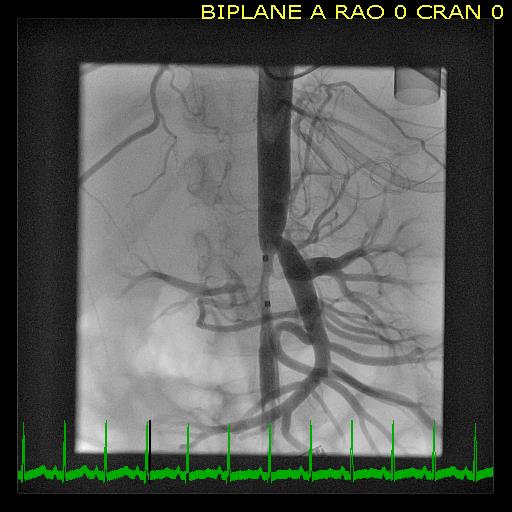
Back to 2019 Abstracts
