Iliac Vein Decompression by Arterial Transposition after Wall Stent Removal for Refractory Pelvic Pain in May Thurner Syndrome
George C Pontikis, Carlos Timaran
UT Southwestern Medical Center, Dallas, TX
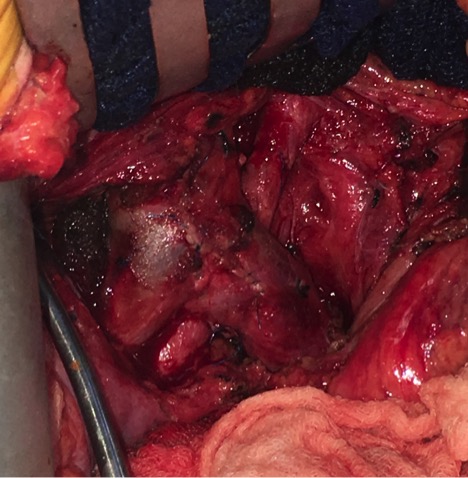
INTRODUCTION: May Thurner Syndrome (MTS) is characterized by a venous outflow obstruction of the left common iliac vein (LCIV) secondary to compression by the overlying right common iliac artery (R CIA) anteriorly and the lumbar spine posteriorly. The spectrum of presentation varies with some patients asymptomatic and others with venous thrombosis resulting in chronic venous hypertension and post-thrombotic syndrome. Fortunately, this disease process can be treated with endovascular stent placement that has demonstrated excellent long-term patency and relatively low risk. A rare entity of pelvic pain after wall stent placement has been described in the literature. This may be a result of extensive oversizing of the stent and the intense inflammatory reaction that ensues to the retroperitoneum and adjacent sacral nerves. Gloviczki et al. described a technique with removal of the wall stent via extraction of the individual wires through small puncture wounds in the vein wall. Following the procedure, there was moderate recurrent compression of the left common iliac vein (CIV) but no evidence of occlusion and no lower extremity symptoms. METHODS: We present a similar case with persistent pelvic pain secondary to prior wall stent placement. After successful removal of the stent by the aforementioned technique, she was noted to have MTS recurrence with complete obstruction of the left CIV relieved with elevation of the artery during intraoperative venography. Given her young age and the severity of her initial MTS symptoms, we felt it prudent to perform a reconstruction that would alleviate this compression while avoiding further manipulation of the venous system. RESULTS: After careful consideration, we proceeded with posterior transposition of the arterial system. The RCIA was fully mobilized, transected and tunneled posteriorly with reconstruction in end-to-end fashion. Repeat venography demonstrated complete resolution of the LCIV compression. The patient recovered well without complications and endorsed complete resolution of her pain and numbness with no recurrence of her prior MTS swelling or pain. CONCLUSIONS:Our case echoes the findings suggested by previous studies in recognizing the incidence of pelvic pain syndrome after prior wall stent placement. Various patient factors should be taken into account prior to proceeding with such aggressive therapies including age, medical comorbidities, and severity of prior MTS symptoms. When proceeding with such interventions, it is important to consider multimodality treatment with the hope of ameliorating their pain and preventing future MTS recurrence. R CIA transposition can be performed safely at the time of stent removal with excellent venographic results demonstrating immediate relief of the extrinsic venous compression. 
Back to 2019 Abstracts
