TransCarotid Artery Revascularization is Associated with Favorable Outcomes in the Treatment of Restenosis After Prior Carotid Endarterectomy
Nadin Elsayed, Ganesh Ramakrishnan, Isaac Naazie, Sharvil U. Sheth, Mahmoud B. Malas
University of California San Diego, San Diego, CA
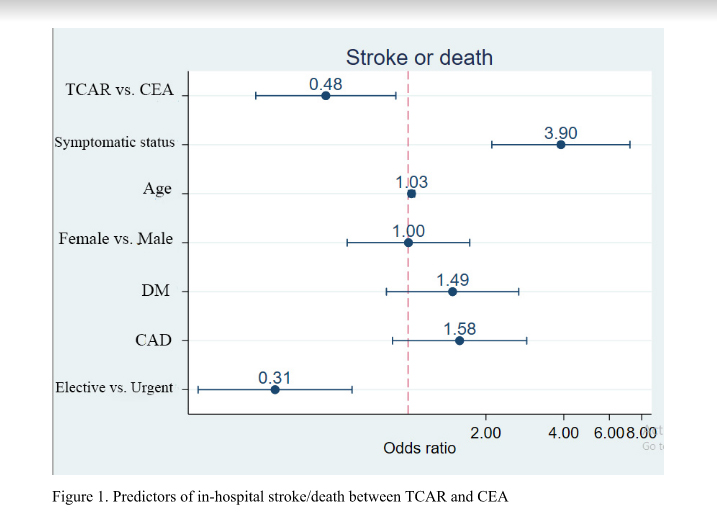
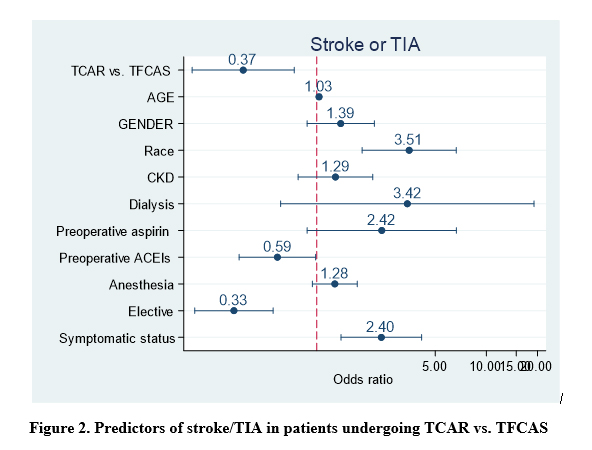
Background: Restenosis after CEA is associated with an increased risk of ipsilateral stroke. However, the optimal treatment modality for this indication has yet to be determined. Here, we evaluate the in-hospital outcomes of transcarotid artery revascularization (TCAR), redo-carotid endarterectomy (CEA), and transfemoral carotid artery stenting (TFCAS) in a large contemporary cohort of patients who underwent treatment for restenosis after CEA. Methods: We performed a retrospective analysis of all patients in the Vascular Quality Initiative database who underwent TCAR, redo-CEA, or TFCAS after ipsilateral CEA between September 2016 and April 2020. Patients with prior ipsilateral CAS, concomitant procedures, and dissection/traumatic lesions were excluded from this analysis. In-hospital stroke, death, stroke/TIA, stroke/death, and stroke/death/MI after TCAR vs CEA and TCAR vs TFCAS were evaluated using multivariate regression analysis.Results: A total of 4,425 patients were available for this analysis. There were 963 (21.8%) CEA, 1,786 (40.4%) TFCAS, and 1,676 (37.9%) TCAR. Patients undergoing TCAR were older and less likely to be symptomatic compared to CEA patients. Both TCAR and TFCAS patients had more CAD and were more likely to have >80% stenosis and to be on dual antiplatelet therapy than CEA patients. TCAR was associated with lower odds of in-hospital stroke/death (OR: 0.48, 95%CI: (0.26-0.9), P=0.021) (Figure 1), stroke (OR: 0.46, 95%CI: (0.23-0.93),P=0.03), MI (OR: 0.32, 95%CI: (0.14-0.73), P=0.007), stroke/TIA (OR: 0.42, 95%CI: (0.24-0.74), P=0.002), and stroke/death/MI (OR: 0.41, 95%CI: (0.24-0.70), P=0.001) when compared to redo-CEA. There was no significant difference in the odds of death between the two groups (OR: 0.99, 95%CI: (0.28-3.5), P=0.995). TCAR was also associated with lower odds of stroke/TIA (OR: 0.37, 95%CI: (0.18-0.74), P=0.005) when compared to TFCAS (Figure 2). There was no significant difference in the odds of stroke (0.56, 95%CI: (0.31-1.03), P=0.066), death (OR:0.82 (95%CI: 0.16-4.3), P=0.81), MI (OR:2.25, (95%CI: 0.8-6.4), P=0.127), stroke/death (OR: 0.64 (95%CI: 0.38-1.06), P=0.09), or stroke/death/MI (OR: 0.68 (CI: 0.43-1.07) P=0.096) between TCAR and TFCAS. Conclusion: TCAR was associated with significantly lower odds of in-hospital stroke, MI, stroke/TIA, stroke/death, and stroke/death/MI when compared to redo-CEA and lower odds of in-hospital stroke/TIA when compared to TFCAS. Additional long-term studies are warranted to establish the role of TCAR as the first line procedural therapy for the treatment of restenosis after CEA.
Back to 2021 Abstracts