Cumulative Financial Impact of the COVID-19 Pandemic on an Academic Vascular Surgery Division
Clayton J. Brinster, G. Thomas Escousse, Ross Parkerson, Charles Leithead, Hernan A. Bazan, Samuel Money, W. C. Sternbergh, III
Ochsner Clinic Foundation, New Orleans, LA
BACKGROUND: The COVID-19 pandemic has fundamentally changed the current health care environment, and the financial and clinical impact of these changes continues to evolve. After an early period of widespread resource redeployment and mandated cancellation of non-emergent procedures in March and April 2020, restrictions on elective cases were subsequently lifted and practices permitted to function without limitation. The Medicare Coronavirus Aid, Relief, and Economic Security Act (CARES) estimated a total financial loss during this interval of -7% to -15% with most health systems already functioning at slim to negative net financial margins. We sought to examine the continuing impact and evolution of these changes within a vascular surgery division at a tertiary medical center.
METHODS: De-identified financial, operating room, vascular laboratory and outpatient clinical records at a single institution were examined retrospectively. Given that restrictions on elective surgery were implemented in early March 2020 and lifted in late April 2020, two intervals were established for comparison: a 14-month control period from January 2019 through February 2020, or Pre-COVID, and March through July 2020, or COVID. Monthly data regarding operative and outpatient clinic volume, financial returns and margins, insurance payor mix, and relative value unit (RVU) generation were recorded and respective trends analyzed.
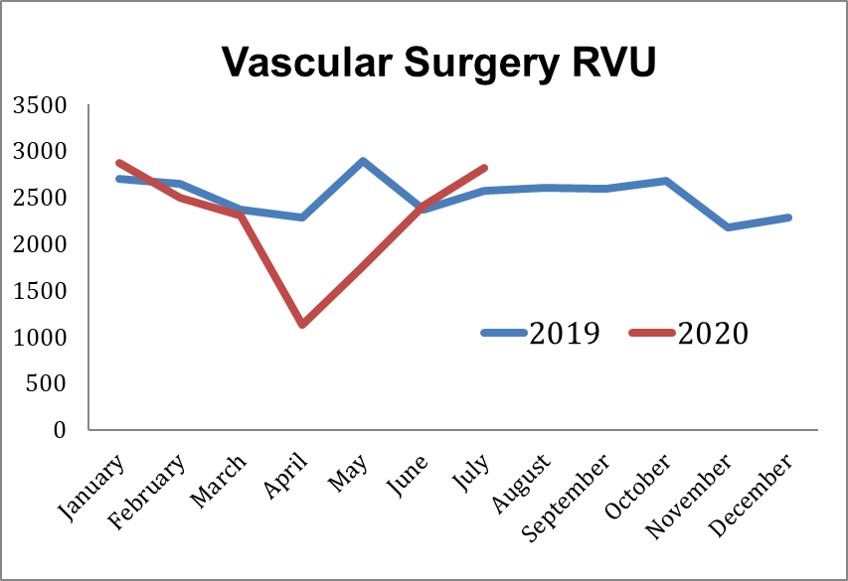
RESULTS: When pre-COVID and COVID intervals were compared, vascular surgery operative volume during the COVID period decreased from 108.1 to 83.5 cases/month (-22.7%), with decreased monthly outpatient encounters, 348.5 to 268.0/month (-23%), and vascular laboratory study volume, 1483.7 to 1029.5/month (-30.6%). Average RVU production decreased from 2506.4 to 2031.7/month (-19%), and total monthly financial return decreased from ,450 to ,000/month (-31.5%). Total divisional financial loss during the COVID period was -,250. Payor mix did not change significantly between the two groups, with 77% Medicare, 15% Commercial and 8% Medicaid pre-COVID versus 74%, 16% and 9%, respectively, in the COVID period. Respective monthly values in the COVID period demonstrate an ongoing, progressive recovery to date in RVU (Figure). Based on monthly averages in 2019 and the total losses recorded during COVID 2020, financial extrapolation modeling predicts that a sustained increase in both case volume and financial return of +5%/month for 32 months or +10%/month for 17 months over pre-COVID values would be required to fully recover pandemic related losses without federal subsidy.
CONCLUSIONS: The COVID pandemic has had a severe nationwide impact on healthcare delivery and reimbursement. Our results demonstrate sustained decreases in operative and outpatient clinical volume and associated financial loss throughout the COVID period, with recovery to pre-COVID monthly financial margins just beginning. Extrapolation from the available data predicts that even aggressive monthly overages of 5 to 10% in clinical production and salutary return would take years to achieve financial equipoise given the sustained decreases already suffered in 2020. Based on this data, Medicare predictions of financial loss and required CARES Act supplementation may be grossly underestimated.
Back to 2021 Abstracts