Back to 2016 Annual Meeting Program
An Integrated Approach to Thoracoabdominal Aortic Aneurysm Repair: Complimentary Roles of Open and Hybrid Approaches
Ehsan Benrashid1, Hanghang Wang1, Nicholas D Andersen1, Jeffrey E Keenan1, Richard L McCann2, George C Hughes1
1Division of Cardiovascular and Thoracic Surgery, Department of Surgery, Duke University Medical Center, Durham, NC;2Division of Vascular Surgery, Department of Surgery, Duke University Medical Center, Durham, NC
Background: Thoracoabdominal aortic aneurysm (TAAA) repair remains a significant clinical challenge. Patients with TAAA are frequently elderly with multiple comorbidities, making decisions regarding whether to offer repair difficult. A hybrid approach utilizing visceral debranching with endovascular aneurysm exclusion has been utilized by some groups, including our own, as a means to treat higher risk patients and therefore allow repair in more patients. However, limited data exists regarding long-term outcomes with this procedure as well as comparison to conventional open repair. As such, the current study describes our institutional integrated approach to TAAA repair utilizing both open and hybrid techniques.
Methods: N = 165 patients who underwent TAAA repair between July 2005 and August 2015 were identified from a prospectively maintained institutional aortic surgery database. Hybrid TAAA repair with complete visceral debranching and endovascular aneurysm exclusion was performed in n = 81 patients, while n = 84 patients underwent conventional open TAAA repair.
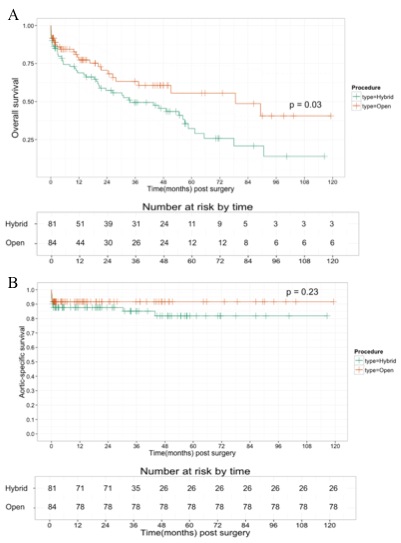
Results: Patient demographics are listed in the Table. Patients in the hybrid repair group were significantly older, more frequently female, and less likely to have a connective tissue disorder or undergo repair for a chronic dissection indication. Hybrid patients also had a generally greater comorbid disease burden, including significantly more chronic kidney disease. Despite the apparently older and sicker cohort, there was no difference in in-hospital mortality between the two-groups (9.9% hybrid vs. 7.1% open; p = 0.59). Major morbidity rates did differ by procedure with patients undergoing open repair having a significantly higher rate of postoperative stroke (9.5% open vs. 0% hybrid; p = 0.017), while patients undergoing hybrid repair had a higher rate of new permanent dialysis (14.8% hybrid vs. 2.6% open; p = 0.043). There was no difference between groups in the rate of postoperative permanent paraplegia/paresis (8.3% open vs. 7.4% hybrid; p = 0.294). One-year survival (Figure 1A) was similar between groups at 69% in the hybrid cohort vs. 77% in the open group. Long-term survival was significantly worse in the hybrid group (5-year survival 32% hybrid vs. 56% open), although late survival appeared to be influenced mainly by comorbid disease burden given the similar long-term aorta-specific survival between groups (Figure 1B).
Conclusions: Use of an algorithmic approach whereby higher risk patients with TAAA are treated using a hybrid approach and lower risk patients with conventional open repair yields satisfactory short and long-term outcomes. The availability of multiple options for TAAA repair within a single center likely allows repair in more patients with consequent decrease in the risk of aorta-related death. 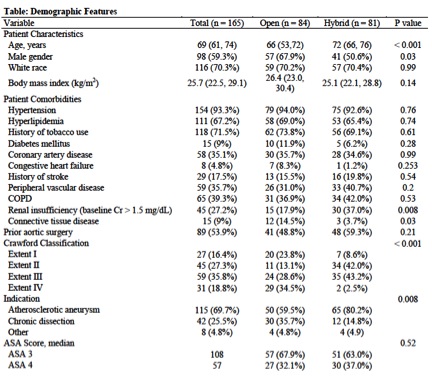
Back to 2016 Annual Meeting Program
