Back to 2016 Annual Meeting Program
Use of Hyperspectral Imaging to Assess Vascular Dysfunction in Arterial Disease
Brandon Sumpio, Jason Chin, Gianluca Citoni, Bauer Sumpio
Yale University School of Medicine, New Haven, CT
INTRODUCTION:
Ultrasound measurement of brachial artery flow mediated dilation during reactive hyperemia has been widely used in research as a non-invasive measure of endothelial function. However, the need for B-mode ultrasonography to measure brachial artery diameter can be technically challenging and inconvenient for providers and patients. Hyperspectral imaging (HSI) is a technology that with limited training can noninvasively measure oxyhemoglobin (oxyHb) and deoxyhemoglobin (deoxyHb) concentrations in the skin to create an oxygenation map. The aim of this pilot study was to determine if HSI could be used to demonstrate vascular dysfunction in the upper extremity of patients with peripheral artery disease (PAD) and coronary artery disease (CAD).
METHODS:
This prospective study included consecutive, consented patients presenting to the vascular clinic with and without diagnosed arterial disease as well as healthy volunteers. Patients underwent HSI at the right bicep, forearm, and palm before and after cuff occlusion (50 mmHg above systolic) for 5 minutes. Patients with blood pressure differences between arms above 15mmHg indicating possible vascular disease in the measured extremity were excluded. The absolute and percent changes in oxyHb and deoxyHb levels were assessed. Medical records of enrolled patients were reviewed for demographic data, medications, surgical history, and other pertinent information. Patients were separated into healthy control and disease (consisting of patients with PAD or CAD) groups. Results are mean +/- SE. Baseline differences in categorical variables of medical history were evaluated using the chi-square and Fisher exact test. Differences in HSI values between the groups were evaluated using the two-tailed t- test with statistical significance determined as P<0.05.
RESULTS:
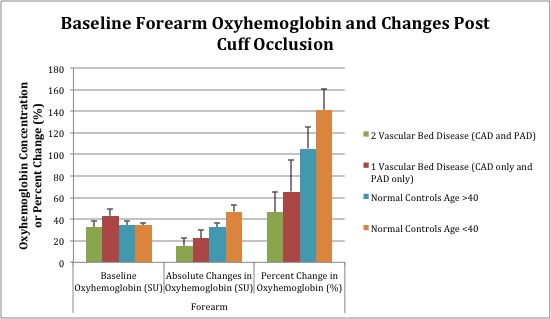
The study enrolled 20 normal controls, including vascular clinic patients without arterial disease as well as healthy volunteers; and 15 disease patients. The distinct groups had similar values at baseline. Significant differences were noted in every area of the arm tested for absolute changes in oxyHb values after cuff occlusion (P<0.05) with the greatest difference noted in the forearm (percent change oxyHb 57% vs 125% [P = 0.005] for disease versus control, respectively) as shown in Table 1. No differences were noted for deoxyHb values. There were no differences between younger (age 40 years) and older control patients. Subgroup analysis of pts with PAD and/or CAD in Figure 1 demonstrated decreasing arterial reactivity (change in oxyHb after occlusion) with increasing number of vascular beds affected.
CONCLUSIONS:
This study presents a novel way to measure endothelial dysfunction similarly to the brachial artery reactivity test. Our results suggest the ability of HSI (using forearm oxyHb changes after suprasystolic brachial cuff occlusion) to assess the presence and severity of PAD and CAD based on systemic vascular dysfunction at sites remote from the clinically diseased vascular bed. This could enable early screening and tracking of arterial disease patients prior to development of clinically advanced disease.
| Disease (n=15) | Control (n = 20) | P-value | ||
| Bicep | Absolute Change OxyHb | 44+/-5 | 69+/-4 | 0.000 |
| Bicep | % Change OxyHb | 166+/-34 | 218+/-18 | 0.195 |
| Forearm | Absolute Change OxyHb | 19+/-5 | 41+/-4 | 0.003 |
| Forearm | % Change OxyHb | 57+/-18 | 125+/-14 | 0.005 |
| Palm | Absolute Change OxyHb | 11+/-4 | 20+/-3 | 0.048 |
| Palm | % Change OxyHb | 18+/-7 | 30+/-5 | 0.168 |
Back to 2016 Annual Meeting Program
