Back to 2016 Annual Meeting Program
Initial in-vitro and in-vivo evaluation of a self-monitoring “smart” bypass graft
Richard F Neville, Samit Gupta, David Kuraguntla
George Washington University, Washington, DC
Background: Prosthetic grafts for lower extremity revascularization and dialysis access fail due to hyperplastic stenosis. Revision of failed grafts often requires a more complex procedure with increased morbidity and mortality as compared to an intervention to maintain assisted primary patency. Therefore, routine surveillance is advocated on a regular basis to monitor graft function, but grafts can fail between these episodic examinations. New microchip technology combined with an innovative sensor may offer automated surveillance with real-time assessment of graft function using a cloud-based algorithm. We performed proof of concept experiments using in vitro and in vivo models to assess the feasibility such a surveillance system.
Methods: A “smart graft” system was evaluated consisting of a prosthetic graft, microelectronics (comprised of a sensor, battery and microprocessor), external monitor and remote processor. The microelectronics were integrated with a PTFE bypass graft without any luminal impact to the graft configuration. The grafts were then placed in a pulsatile, recirculating flow system to approximate physiologic conditions. Hemodynamic parameters were varied in this pulsatile system to assess real-time flow properties in an in vitro model. Custom stenoses were created and inserted into the in vitro model in order to mimic reduced diameters both proximal and distal to the grafts. After initial data was gathered, the “smart graft” system was studied in a sheep model to assess proof of concept in vivo.
Results: The in-vitro flow model demonstrated the ability of the system to determine multiple factors related to prosthetic graft function with various hemodynamic flow conditions. Data analysis was able to successfully determine parameters such as flow rate and changes in flow velocity. Waveform analysis was applied to determine an algorithm for each parameter. These algorithms allowed determination of stenosis location (proximal or distal) and degree of stenosis by a remote processor for display on a monitor in real-time. Similarly, the initial in-vivo experiments confirmed the ability of the system to generate data under biologic conditions.
Conclusion: Initial in-vitro and in-vivo experiments have demonstrated the ability for a “smart graft” system to remotely monitor graft function in real-time. This automated system shows promise to deliver real-time data that can be analyzed by cloud-based algorithms which would alert the clinician of stenosis for further diagnostic study or intervention prior to graft failure. 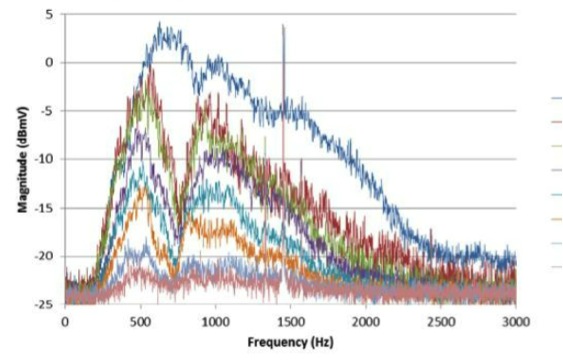
Back to 2016 Annual Meeting Program
