Back to 2016 Annual Meeting Program
The Physician Quality Reporting System (PQRS) Successfully Measures Quality of Care for Elective Procedures for Asymptomatic Abdominal Aortic Aneurysms and Asymptomatic Carotid Artery Disease
Rodney P Bensley1, Salvatore T Scali1, Kristina A Giles1, Javairiah Fatima1, Thomas S Huber1, Andres Schanzer2, Jack L Cronenwett3, Adam W Beck1
1University of Florida, Gainesville, FL;2University of Massachusetts Medical School, Worcester, MA;3Dartmouth-Hitchcock Medical Center, Lebanon, NH
Background: The Physician Quality Reporting System (PQRS) was developed by CMS to provide financial incentive for reporting outcomes. The SVS proposed PQRS measures pertaining to treatment of asymptomatic patients with small AAAs or carotid occlusive disease. These PQRS measures use discharge location not to home and long length of stay (LOS) (available from claims data) as proxies for likely post-operative complications. We sought to validate these PQRS measures within the Vascular Quality Initiative (VQI) by determining if they are associated with post-operative major complications, as well as 1-year mortality, which could indicate futility of the initial prophylactic operation.
Methods: The VQI database was used to identify all patients undergoing elective EVAR or open AAA repair (oAAA) of AAAs <6cm in men and <5.5cm in women, or asymptomatic carotid revascularization (CAS or CEA). PQRS measure LOS thresholds were ≤ 2 days for EVAR, ≤7 days for oAAA, and ≤ 2 days for CAS or CEA. The proportion of patients meeting these LOS thresholds and discharge to home was determined. The postoperative complication rate, 30-day mortality rate, and 1-year mortality rate were stratified by whether or not these measures were met.
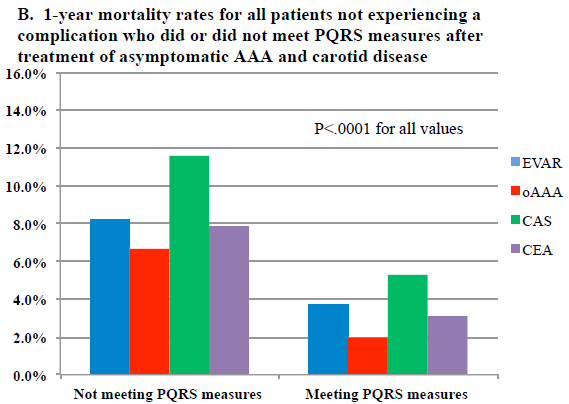
Results: Between 2003 and 2014, 9,619 EVAR, 2,191 oAAA, 3,423 CAS, and 27,593 CEAs were performed electively for asymptomatic disease. The majority of patients (83%) met the PQRS measures evaluated (Table). Failure to meet PQRS measures was most commonly due to prolonged LOS (94%), rather than discharge disposition other than home (26%). Overall, the incidence of postoperative complications was significantly higher in patients not meeting PQRS measures (22.8% vs. 3.4%, P<.0001) and this effect was seen for each procedure subtype. 30-day (3.1% vs. 0.3%, P<.0001) and 1-year mortality rates (11.7% vs. 3.4%, P<.0001) were also significantly higher in all patients not meeting PQRS measures and in each procedure subtype (Figure 1A). After excluding patients with any postoperative complications, 1-year mortality remained significantly higher in patients not meeting the PQRS measures (Figure 1B).
Conclusion: SVS-proposed PQRS measures correctly identify higher post-operative complication rates using claims data. Failure to meet these PQRS quality measures is associated with higher rates of postoperative complications, 30-day, and 1-year mortality after elective AAA repair and treatment of asymptomatic carotid disease, where proper patient selection is required to avoid complications and unhelpful procedures. One-year mortality was significantly higher when these PQRS measures were not met, suggesting the likelihood of poor patient selection. These PQRS measures appear appropriate for comparing care across centers. 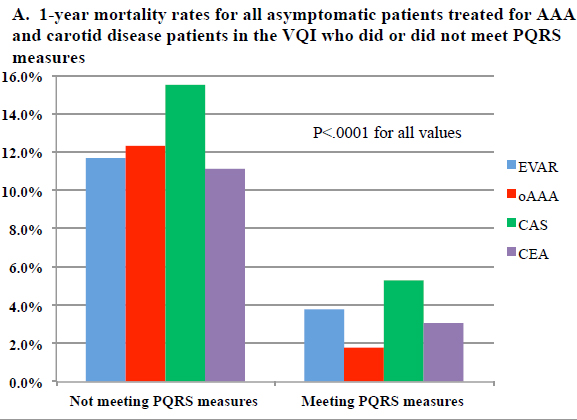
| Procedure | Proportion Meeting PQRS Measures | Reason for failure to meet measure | Reason for failure to meet measure | Postoperative complications | 30-day Mortality |
| (Total N) | % (N) | LOS | D/C status | (Not meeting vs. meeting) | (Not meeting vs. meeting) |
| EVAR (n=9619) | 78% (7504) | 96% | 21% | 18.4% vs. 2.3%, P<.0001 | 2.5% vs. 0.2%, P<.0001 |
| oAAA (n=2191) | 60% (1324) | 86% | 43% | 40.0% vs. 5.9%, P<.0001 | 5.1% vs. 0.2%, P<.0001 |
| CAS (n=3423) | 87% (2965) | 92% | 29% | 21.0% vs. 1.1%, P<.0001 | 4.6% vs. 0.4%, P<.0001 |
| CEA (n=27,953) | 86% (23,695) | 94% | 24% | 21.6% vs. 3.9%, P<.0001 | 2.8% vs. 0.3%, P<.0001 |
Back to 2016 Annual Meeting Program
