Back to 2016 Annual Meeting Posters
Factors Affecting Deep Venous Thrombosis Following Endovascular and Open Abdominal Aortic Aneurysm Repair
Matthew D'Alessandro, Jonathan Schor, Chenee Tyson, Kuldeep Singh, Jonathan Deitch, Saqib Zia
Staten Island University Hospital, Staten Island, NY
OBJECTIVES
Identifying factors that contribute to deep venous thrombosis (DVT) after surgery can help us recognize which patients will require extra resources earlier in their stay, and allow us to anticipate their needs and potential complications. The objective of this study was to compare the patients that underwent endovascular abdominal aortic aneurysm repair (EVAR) to patients who had an open repair to identify factors contributing to development of deep venous thrombosis.
METHODS
We reviewed all EVAR and open abdominal aortic aneurysm (AAA) operations reported to the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) from 2005 to 2011 and identified all of the patients who had a concomitant DVT. Ruptured cases as well as patients with the diagnosis of cancer were excluded. Patient demographics, procedural characteristics, and postoperative complications were reviewed. The patients were divided into “EVAR” and “Open” subgroups based on the procedure performed. Predictors for development of DVT were identified by multivariate analysis.
RESULTS
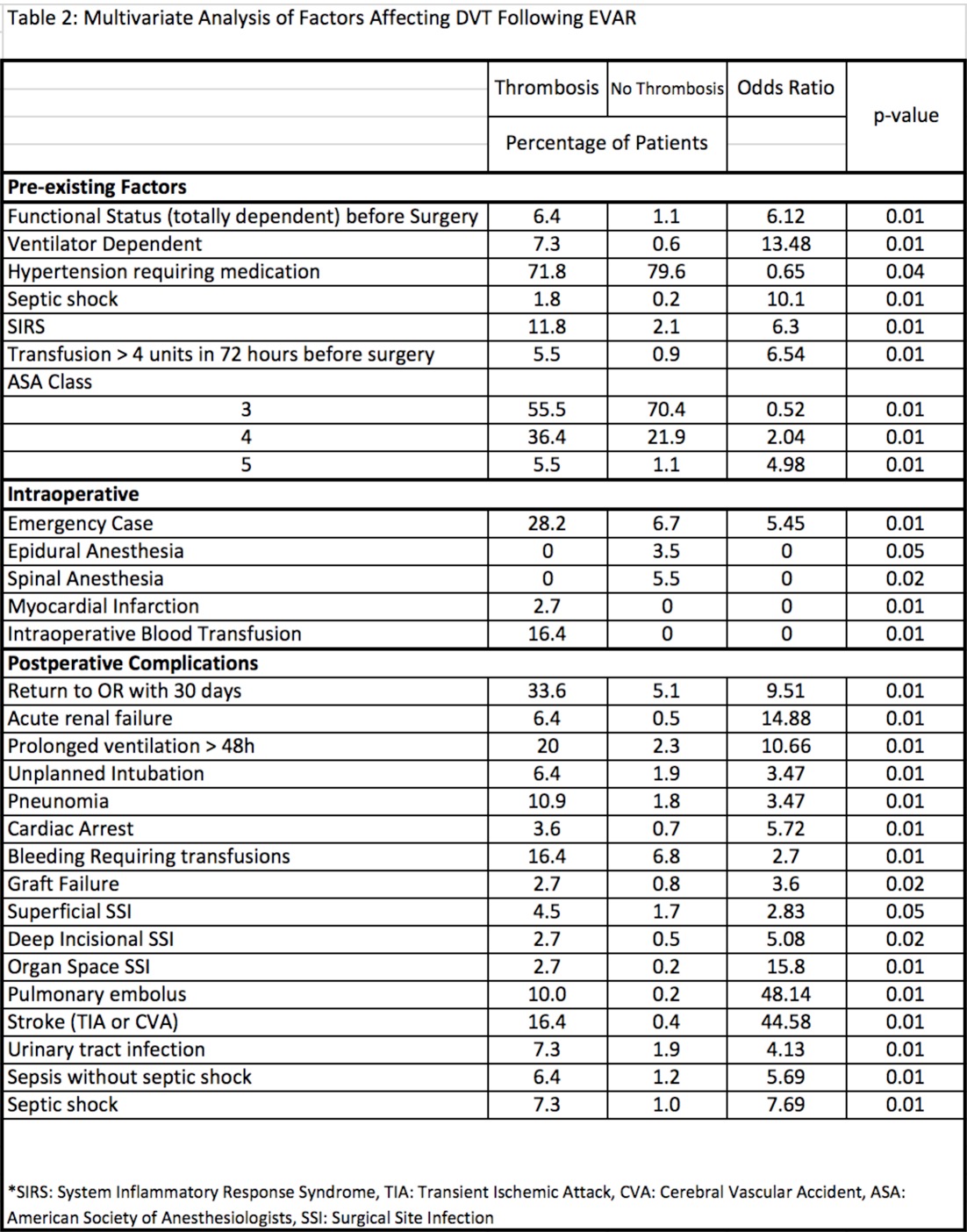
The cases reviewed were divided into an EVAR subgroup, composed of 17,046 patients, and an Open subgroup, composed of 5,706 patients. In the EVAR group, 90 patients were found to have a DVT, while in the Open group, DVT was found in 74 patients. Increased likelihood of thrombosis in the EVAR group vs the Open group was seen in patients with age >80 years (31.1% vs 4.1%, p=0.0001). Factors that were associated with thrombosis in the Open group were prolonged ventilation greater than 48 hours (47.3% vs 13.3%, p=0.0001), unplanned postoperative intubation (21.6% vs 6.7%, p=0.01), development of postoperative pneumonia (25.7 vs 5.6%, p=0.0007), postoperative myocardial infarction (5.4% vs 0%, p=0.03), presence of postoperative bleeding that required transfusion (27% vs 13.%, p=0.05), presence of postoperative sepsis (20.3% vs 4.4%, p=0.004) and postoperative septic shock (16.2% vs 5.6%, p=0.05). The Open and EVAR groups were also analyzed independently to identify factors affecting thrombosis (Table 1 & Table 2). Multiple factors were found to be significant for development of DVT in the EVAR group, but not in the Open group. These included the presence of preoperative hypertension, septic shock, pre and postoperative transfusion, postoperative acute renal failure, graft failure, superficial and deep surgical site infections.
CONCLUSIONS
Various pre-operative characteristics and postoperative complications were identified as having a significantly higher occurrence in patients who developed a DVT after having undergone an open versus an endovascular AAA repair. In general, the Open thrombosis group had more postoperative complications while the EVAR group had more advanced age. Overall, factors relating to respiratory complications such as pneumonia and prolonged ventilation were associated with the greatest odds of having a concomitant DVT. Interestingly, many of these factors were found to only be significant in EVAR cases. 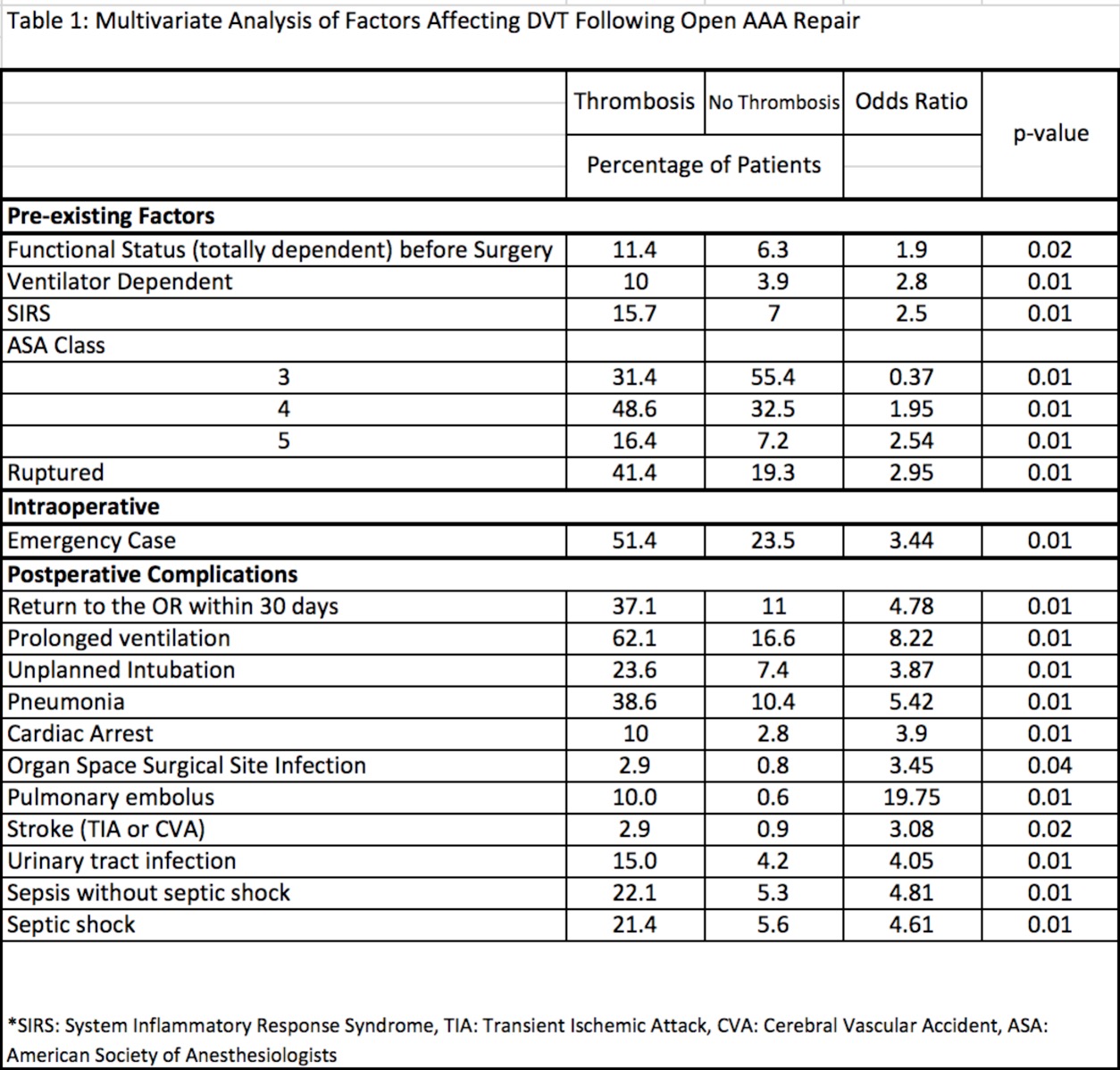
Back to 2016 Annual Meeting Posters
