Persistent Underrepresentation of Female Patients in US Trials of Common Vascular Diseases Since 2008
Jessica Mayor, Ourania Preventza, Joseph L. Mills, Sr., Miguel Montero-Baker, Ramyar Gilani, Zachary Pallister, Jayer Chung
Baylor College of Medicine, Houston, TX
INTRODUCTION: Women have been historically underrepresented in vascular surgery and cardiovascular medicine trials. The rate and change in representation of women in trials of common vascular diseases over the last decade is unknown.
METHODS: We used publicly available data from ClinicalTrials.gov to evaluate trials pertaining to carotid artery stenosis (CAS), peripheral arterial disease (PAD), thoracic and abdominal aortic aneurysms, and Type B aortic dissections from 2008 to the present. We evaluated representation of women in these trials based upon participation-to-prevalence ratios (PPR), which are calculated by dividing the percentage of women among trial participants by the percentage of women in the disease population. Values of 0.8-1.2 reflect similar representation.
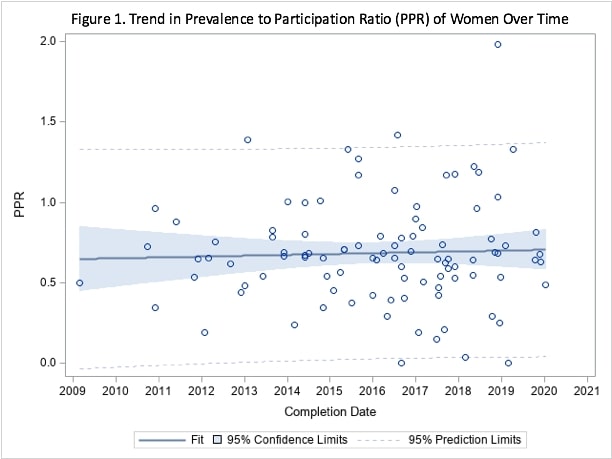
RESULTS: All 98 trials reported sex distribution. There were 11 CAS trials, 69 PAD trials, 16 aortic aneurysm trials, and 2 Type B dissection trials. The total number of participants in these trials was 41,622 with a median number of participants per trial was 150.5 (IQR 50, 252). The percentage of women in the disease population was 51.9% for CAS, 53.1% for PAD, 34.1% for aortic aneurysm, and 30.9% for Type B dissection. Industry-sources funded 76 (77.6%) of trials, while the Veteranís Affairs Administration (4; 4.1%), unspecified University (7; 7.1%) and extramural (11; 11.2%) funded the remainder. The overall median PPR for all four diseases was 0.65 (IQR 0.51, 0.80). Women were underrepresented for all four conditions studied [CAS: 0.73 (IQR 0.62, 0.96); PAD: 0.65 (IQR 0.53, 0.77); aortic aneurysm: 0.59 (IQR 0.38, 1.20); Type B dissection: 0.74 (IQR 0.65, 0.84)]. There was no significant difference in PPR among the diseases (p = 0.88). From 2008 to the present, there was no significant change in PPR values over time overall (r2=0.0015; p = 0.70; Figure 1). When examined individually, PPR did not change significantly over time for any of the disease studied (for each, r2 < 0.04; p > 0.45). PPR did not vary significantly over time for any of the funding sources (for each, r2 < 0.85, p > 0.08). There was appropriate representation (PPR 0.8-1.2) in a minority of trials for each disease except Type B dissection (CAS: 27.3%, PAD: 15.9%, aortic aneurysm: 18.8%, Type B dissection: 50%). Trials that were primarily funded from university sources had the highest median PPR (1.04; IQR, 0.21, 1.27), followed by industry-funded (0.67; IQR 0.54, 0.81); and extramurally-funded (0.60; IQR 0.34, 0.73). Studies funded by Veterans Affairs had the lowest PPR (0.02, IQR 0.00, 0.11; p = 0.004). CONCLUSIONS: Participation of women in US trials of common vascular diseases remains low and has not improved over time since 2008. Therefore, the generalizability of recent trial results to female vascular patients remains unknown. Improved understanding of the etiology for poor female trial participation, advocacy, and education are required to improve generalizability of trial results for female vascular patients.
Back to 2021 Abstracts