Decreased Cases of Acute Stroke and Increased Deaths at Home in an Epicenter of the COVID-19 Pandemic
Clayton J. Brinster, Thomas Hawken, Gabriel Vidal, Ross Parkerson, Charles Leithead, Hernan A. Bazan, Samuel Money, W.C. Sternbergh, III
Ochsner Clinic Foundation, New Orleans, LA
BACKGOUND: The COVID-19 pandemic has fundamentally changed the healthcare landscape in New Orleans (NOLA), which demonstrated one of the highest early per capita rates of COVID infection in the United States. The evolving national impact of the pandemic on medical care for conditions other than COVID-19 has been difficult to quantify, and delayed care for life-threatening, acute conditions has been sporadically reported. We examined the impact of the COVID pandemic on acute stroke care at a tertiary medical center with a comprehensive stroke referral network.
METHODS: Acute stroke admissions, transfers, “telestroke” consults, and interventional stroke therapies, including urgent carotid endarterectomy and stenting, intracranial embolization, aspiration thrombectomy, and tissue plasminogen activator administration, between January 2019 and July 2020 were identified and two cohorts established: January 2019 through February 2020 (Pre-COVID) and March 2020 through July 2020 (COVID). NOLA Emergency Medical Services (EMS) data from 2019 and 2020 was formally requested.
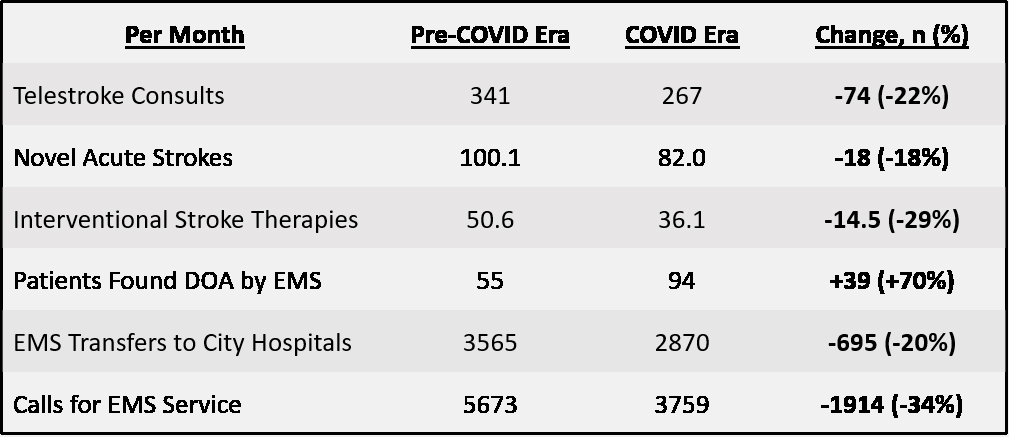
RESULTS: Overall, total novel acute stroke diagnoses decreased by 18% (100.1/month to 82.0/month) in the COVID era. Interventional stroke therapies decreased from an average of 50.6/month to 36.1/month (-29%) when these cohorts were compared. Telestroke consults decreased from 341/month to 267/month (-22%). Official NOLA EMS data revealed a stark increase in the number of patients found dead at home on ambulance arrival for urgent medical transport (DOA) in the COVID era (94/month vs. 55/month, +70%). In addition, NOLA EMS transferred significantly fewer urgent patients (3565 vs. 2870; -20%) to city hospitals and received fewer calls for emergent service (5673 vs. 3759; -34%) in the COVID era. Analysis of trends during the COVID period demonstrates a return to the pre-COVID rate of acute stroke cases diagnosed (105/month) for June and July 2020, but a sustained, significant decrease in stroke interventions (42/month; -17%) and telestroke consults (294/month; -14%) during the same recent interval.
CONCLUSIONS: During the course of the COVID-19 pandemic in an early national epicenter of infection, we report unanticipated major decreases in cases of acute stroke, interventions for acute stroke, and telestroke consults at a comprehensive stroke referral center. In addition, citywide EMS data demonstrates that significantly fewer patients needing emergent medical attention have been transported to citywide hospitals, and 70% more patients per month have been reported DOA by EMS personnel when called for medical emergency. Although the etiology of these deaths is unknown, this constellation of findings substantiates growing national concern that patients continue to delay care for acute conditions in the COVID era, potentially leading to increased, preventable morbidity and mortality.
Back to 2021 Abstracts