Contemporary Outcomes Of Limb-Salvage Procedures Using VQI-Medicare Linked Data: Racial And Ethnic Disparities Persist
Asma Mathlouthi, Nadin Elsayed, Isaac Naazie, Mahmoud B. Malas, Andrew Barleben
University of California, San Diego, San Diego, CA
Introduction:Several reports have shown that ethnic and racial minorities with chronic limb-threatening ischemia (CLTI) are more likely to undergo major amputation. Whether this disparity is driven by limited access to care, statistical discrimination or biological factors remains a matter of debate. We sought to study the effect of race/ethnicity on short and long-term outcomes of limb-salvage procedures among patients with CLTI.
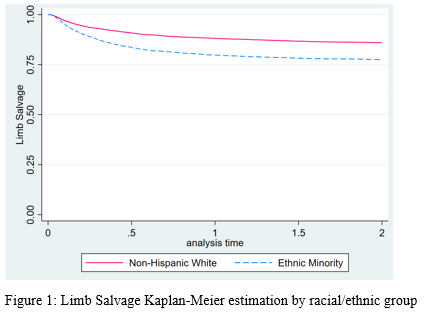
Methods:We identified all patients who underwent first time (open or endovascular) revascularization for CLTI between January 2010 and December 2016 in the VQI-Medicare linked database. These patients were divided into Non-Hispanic Whites (NHW) and Racial/Ethnic minority (REM) groups. Early endpoints included length of stay (LOS) and operative mortality, while 2-year outcomes included major amputation, freedom from subsequent revascularization, number of limb salvage reinterventions and all-cause mortality.Results:Out of 17,228 presenting with CLTI, 69.8% were NHW. REM patients were younger (mean age, 70.1±11.4 years vs. 74.2±10.5 years, P<0.001) and more likely to be females (44.9% vs. 37.7%, P<0.001). Other baseline differences included a higher rate of smoking history, CAD, COPD and CKD among NHW, whereas REM patients were more likely to have diabetes and HTN and more likely to present with tissue loss (78.4% vs. 76.6%, P=0.01). Preoperative ABI and procedure type (endovascular vs. open) were similar between the groups. On multivariable analysis, non-white race/ethnicity was associated with a 13% increase in LOS and a 23% decrease in operative mortality. In regard to 2-year outcomes, limb salvage estimates were 86% for the NHW groups versus 77.5% for the REM group, P<0.001 (Figure 1). NHW patients achieved higher rates of freedom from subsequent revascularization (67.9% vs. 66.6%, P=0.05), but significantly lower rates of overall survival (68.4% vs. 70.2%, P=0.01) when compared to their REM counterparts. Patients in the REM group were more likely to undergo more than two limb-salvage reinterventions during follow-up (13.7% vs. 8.6%, P<0.001). After adjusting for potential confounders, racial/ethnic minority patients had significantly higher odds of major amputation at 2 years [aHR(95%CI): 1.46(1.35-1.6), P<0.001] (Table 1).Conclusions:In this VQI-Medicare matched study, racial and ethnic minority patients continue to face a higher major amputation risk despite having equivalent attempts at limb salvage. Further studies identifying risk factors and evaluating intervention strategies that may be more effective in preventing amputation in this particular population are warranted.
Table 1: Outcomes by racial/ethnic group
| Outcomes | NHW N=12,020 (69.8%) | REM N=5,208 (30.2%) | P-value | aOR | 95%CI | P-value |
| Operative Mortality, N (%) | 441 (3.67) | 129 (2.5) | <0.001 | 0.77 | 0.6-099 | 0.042 |
| LOS , median (IQR) | 4 (1-9) | 6 (1-13) | <0.001 | 1.13 | 1.04-1.24 | 0.004 |
| 2-year Outcomes: | ||||||
| Limb salvage | 86% | 77.5 | <0.001 | 1.46 | 1.35-1.6 | <0.001 |
| Freedom from revascularization | 67.90% | 66.60% | 0.054 | 0.9 | 0.83-0.96 | 0.005 |
| Freedom from ACM | 68.40% | 70.20% | 0.014 | 0.93 | 0.86-1.01 | 0.1 |
| Limb slavage reinterventions> 2, N (%) | 1,033 (8.6) | 713 (13.7) | <0.001 | 0.99 | 0.86-1.13 | 0.9 |
Back to 2021 Abstracts