Cost Analysis of Timing of Carotid Subclavian Revascularization in TEVAR
Hunter M. Ray1, Akshita Kumar2, Jacob J. Siahaan1, Christopher R. Conner2, Kristofer M. Charlton-Ouw1
1Gulf Coast Vascular, Houston, TX, 2UT Health, McGovern Medical School, Houston, TX
INTRODUCTION: Thoracic Endovascular Aneurysm Repair (TEVAR) has become increasingly prevalent in the endovascular era. New advances promise a total endovascular solution for subclavian artery revascularization (SAR), but previous studies failed to analyze the cost effectiveness of such a solution in comparison to carotid-subclavian bypass or transposition (Open SAR) in conjunction with TEVAR. Here we analyze hospital charge data to determine a potential price point for such a solution.
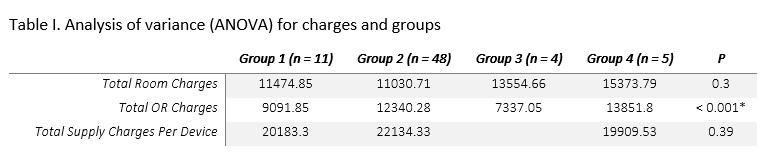
METHODS: Charge data was obtained from one tertiary, urban hospital and included total charges, total room charges, total OR charges and total supply charges. The total supplies charge was adjusted to account for the number of TEVAR devices implanted when appropriate as this was by far the biggest driver of supply cost. Four different combinations of TEVAR and SAR were examined, each with different methods of revascularization and/or timing. The groups investigated were: 1) TEVAR + Open SAR in a single operative setting; 2) TEVAR + Open SAR at different hospital admissions; 3) an investigational single-branched TEVAR; and 4) TEVAR + Open SAR at separate operating room visits but same hospitalization. For group 3, only total room charges and total OR charges were examined given that the investigational device remains premarket without a commercial price. In order to calculate the cost of performing an Open SAR and a TEVAR for group 2, individual isolated TEVAR charges were combined with average isolated Open SAR charges. Analysis of variance and linear regression analysis were used to compare associations with charge data using SAS.
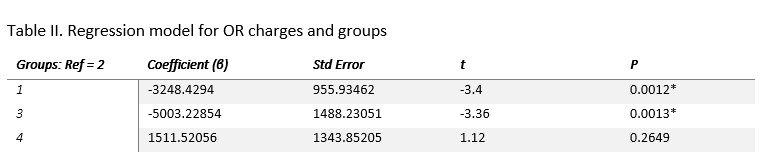
RESULTS: Analysis of variance for each group and charge is shown in Table 1 with total OR charges found to be significant. For our regression model with group 2 as the reference, we found that total OR charges were significantly lower for groups 1 (p=0.0012) and 3 (p=0.0013) compared to group 2. The total OR charges for groups 2 and 4 were not significantly different (Table 2). Total room charges and total supply charges adjusted by number of TEVAR devices (Total supply charge/ device) did not significantly differ between groups (Table 2). Groups 1 and 3 in terms of total OR cost are not significantly different (p=0.2972).
CONCLUSIONS:Based on these findings it appears that the estimated cost is significantly lower when TEVAR and SAR are performed in the same setting. However, total room costs and supply costs per device do not appear significantly different noting that the majority of cost difference appears to be related to OR related costs. In order for a single-branched TEVAR to be cost effective in comparison to TEVAR + open SAR, the device must cost roughly the same price as a standard TEVAR device.
Back to 2021 Abstracts