Improved Perioperative Mortality after Aorto-Enteric Fistula Repair: Lessons Learned from a 20-year Experience
Akeem Bartley, Salvatore T. Scali, Suzanah Patterson, Martin D. Rosenthal, Chasen Croft, Martin S. Back, Dean J. Arnaoutakis, Michol A. Cooper, Gilbert R. Upchurch, Jr., Thomas S. Huber
University of Florida- Gainesville, Gainesville, FL
INTRODUCTION: Aorto-enteric fistula(AEF) are rare but represent one of the most challenging and devastating problems vascular surgeons manage. Over the past twenty years, endovascular techniques have increasingly supplanted open aortic repair further reducing availability of centers and surgeons experienced in AEF management. Several issues surrounding AEF treatment remain unresolved including optimal reconstruction and conduit selection. The purpose of this analysis was to review our experience with AEF and highlight aspects of care that have affected outcomes over time.
METHODS: We performed a single center, retrospective review of all consecutive AEF repairs(1999-2019) and recorded pre-hospital history, patient level factors, operative details and postoperative outcomes. The primary end-point was 30-day mortality. Secondary end-points included incidence of complications and overall survival. We defined major adverse vascular events (MAVE) as any major limb amputation and/or vascular reconstruction failure (occlusion/reoperation/bleeding). Time-dependent comparison of outcomes was completed. Cox proportional-hazards modeling and life-table analysis estimated risk and freedom from end-points when appropriate.
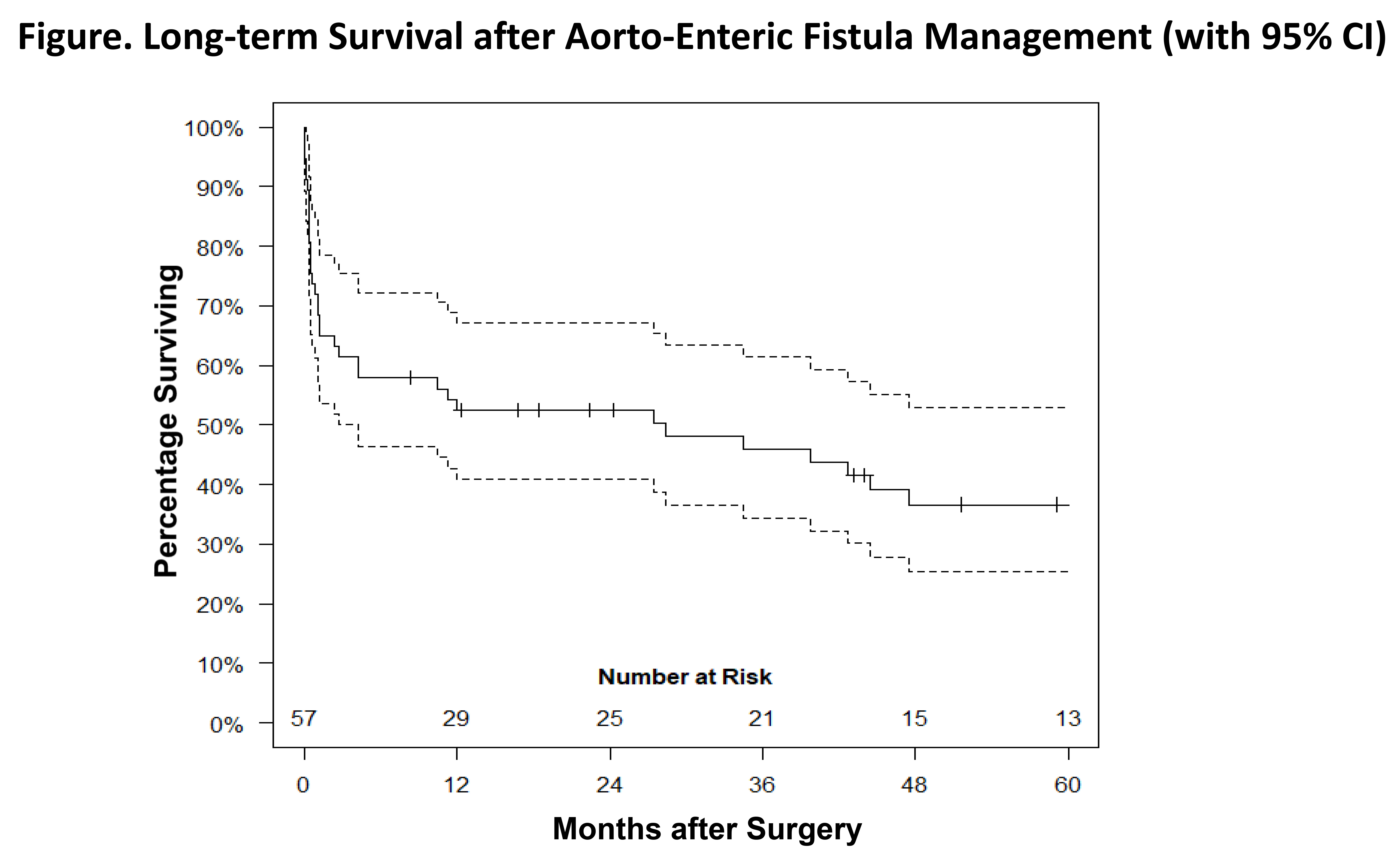
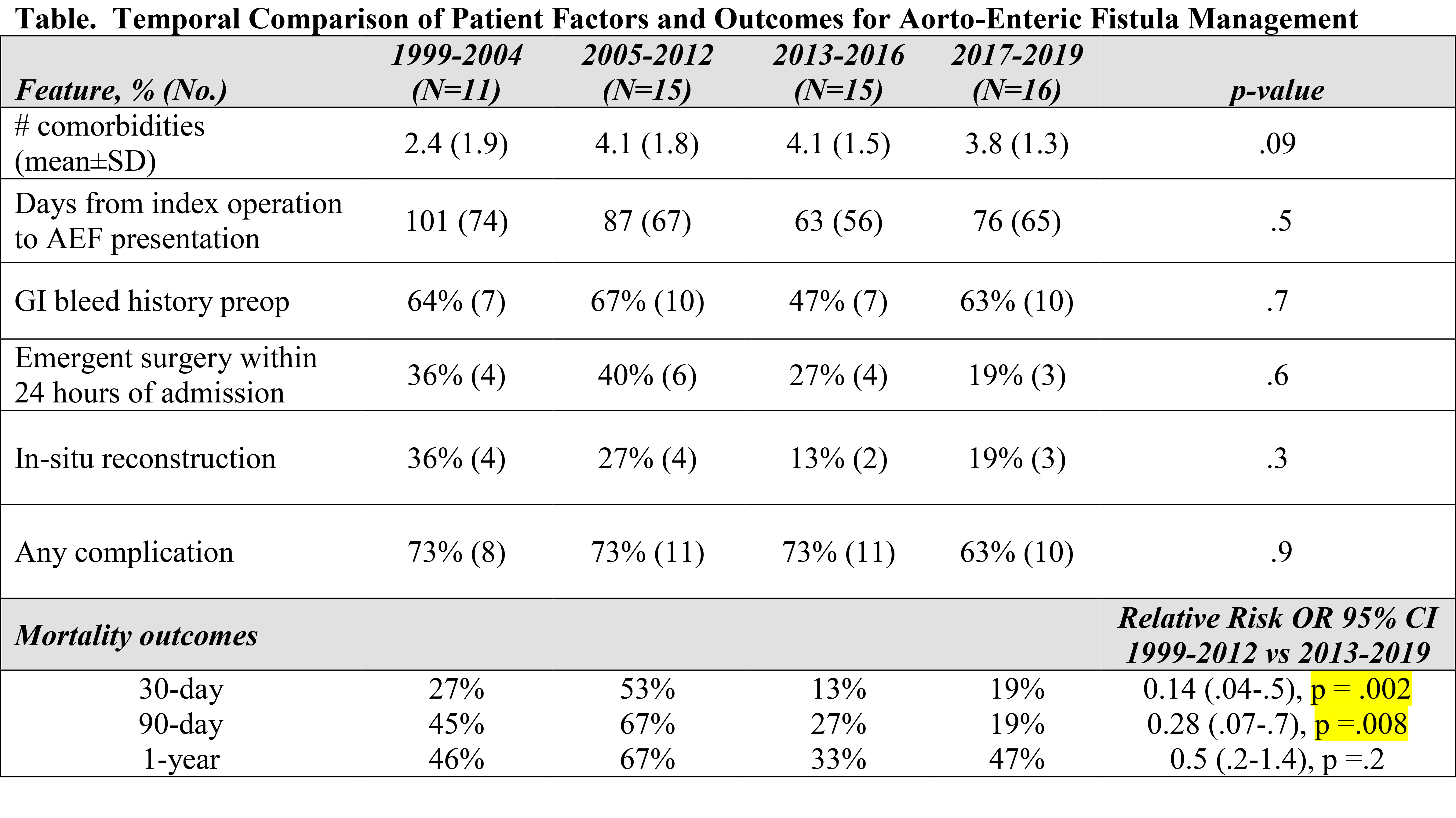
RESULTS: 57 patients (37% female; n=21) presented with AEF and median age was 69 (interquartile range [IQR] 61, 74] years. Median follow-up time was 10 [IQR 3-21] months. The most common presenting symptoms were pre-hospital gastrointestinal bleeding(60%, n=34) and abdominal pain(56%, n=31). For the overall experience, 30%(n=17) underwent extra-anatomic bypass with aortic ligation, 30%(n=17) rifampin-soaked Dacron graft, 26% (n=15) femoral vein (e.g. NAIS), and 14%(n=8) cryopreserved aortic allograft. The enteric communication involved the duodenum in 85%(n=48) and a double layer hand-sewn primary repair was most commonly employed (61%, n=35). 30-day mortality was 35%(n=20) with no significant difference between 90 (39%, n=22) and 180-days (42%, n=24). Morbidity was 70% (n=40) with gastrointestinal (30%, n=17; leak [9%]), pulmonary (25%, n =14), and renal (AKI, 21%) complications being most common. MAVE occurred in 27% (n=15) while incidence of re-operation for any vascular and/or gastrointestinal related complication was 56% (n=32). One-year freedom from MAVE was 70±8% while one and 3-year survival was 54±6% and 48±8%, respectively(Figure). When examining temporal trends in patient presentation and outcomes, significantly improved early survival was evident despite no change in patient factors, operative strategy or morbidity(Table). Pre-hospital history of gastrointestinal bleeding was associated with worse survival (HR 2.0, 95% CI 1.0-3.9; p =.06); however, method of reconstruction (in-situ vs. extra-anatomic), postoperative gastrointestinal or vascular complication, omental flap use and prior EVAR history were not predictive of outcome.
CONCLUSIONS: Improving short-term mortality has occurred despite no significant change in patient presentation or postoperative complications. This highlights increasing institutional experience in selecting the optimal surgical strategy and improved ability to rescue patients experiencing adverse postoperative events. An individualized approach to reconstruction and conduit choice can lead to best outcomes when patients are managed at a high-volume aortic surgery center.
Back to 2021 Abstracts