Migration of high cardiac risk patients from open to endovascular procedures is evident within the Society for Vascular Surgery Vascular Quality Initiative
Juliet Blakeslee-Carter, Zdenek Novak, John Axley, Danielle Sutzko, Graeme McFarland, Benjamin Pearce, Emily Spangler, Marc Passman, Adam Beck
University of Alabama at Birmingham, Birmingham, AL
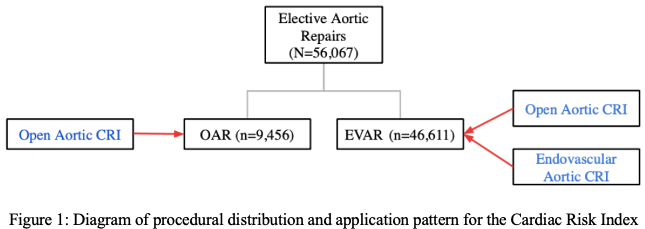
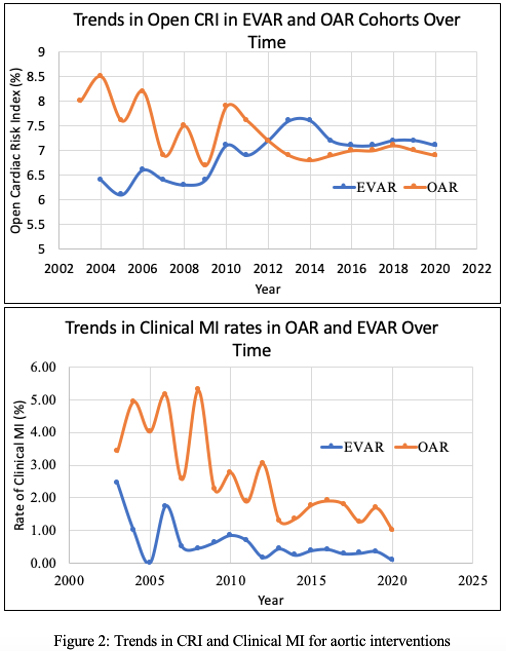
Introduction: While postoperative myocardial infarction (POMI) remains one of the most common complications of vascular procedures, recent studies have shown a decrease in POMI rates following both open and endovascular interventions. This phenomenon, while likely multifactorial, may be attributable to the migration of high-risk patients from open procedures to lower risk endovascular alternatives. If so, trends observed in POMI should be reflected in decreasing pre-operative cardiac risk in open procedures, with higher risk patients undergoing corresponding endovascular treatment. Using Vascular Quality Initiative (VQI) data, a VQI Cardiac Risk Index(CRI) scoring system has been previously validated as a pre-operative assessment. This study aims to identify and correlate trends in VQI CRI for open abdominal aortic aneurysm (OAR) with trends in the CRI for corresponding endovascular aortic repair (EVAR) to support the theory that patient migration is a substantial factor contributing to decreased POMI following open vascular procedures. Methods: A retrospective review of VQI data from 2003-2020 for all patients undergoing elective aortic repairs (OAR and EVAR) was conducted. The CRI developed for the open repair was applied to both the OAR and EVAR cohorts, taking into account appropriate coding of endovascular variables onto an open procedure template (Figure 1). Results: A total of 56,067 elective aortic repairs were identified; 83% were EVAR (n=46,611) and 17% were OAR (n=9,456). Within the OAR cohort, the average open CRI was 7.1%. with significant decrease from 2003 to 2020 (8% ± 4.6% vs 6.9% ± 4.4%, p<0.001), which corresponded to a significant decrease in clinical MI rate (4.1% vs 1.4%, p<0.001)(Figure 2). Over that same time period, within the EVAR cohort, the average open CRI was 7.2% and showed a significant increase (6.6% ± 4.2% vs. 7.2% ± 4.4%, p<0.001). Within the EVAR cohort, the EVAR CRI did not show any significant changes over time (average 0.48%), while the actual rate of clinical MI showed a significant decrease (1.1% vs 0.3%, p=0.002) (Figure 2). Gap analysis was conducted within the EVAR cohort between actual EVAR CRI and theoretical open CRI, which demonstrated that patients within the EVAR cohort would have had an average of 6.7% increase in risk had they undergone an open procedure.Conclusions: In aortic interventions, there was a significant increase in respective open CRI within endovascular procedures and a significant decrease in open procedures. The trends in CRI were supported by decreasing rates of MI within open procedures. These finding support the theory that decreased trends in POMI in open procedures are due to patient selection, with high risk patients being treated with endovascular alternatives, resulting in more high-risk patient features within the endovascular cohort. On average the standard EVAR patient would have a 6.3% increased risk having undergone an open procedure.
Back to 2021 Abstracts