Claviculectomy for Exposure and Repair of Expanding Right Subclavian Artery Aneurysm despite previous Proximal and Distal Ligation
Tiffany R. Bellomo, Scott Robinson, William R. Lynch, Karen M Kim, Matthew A. Corriere
University of Michigan, Ann Arbor, MI
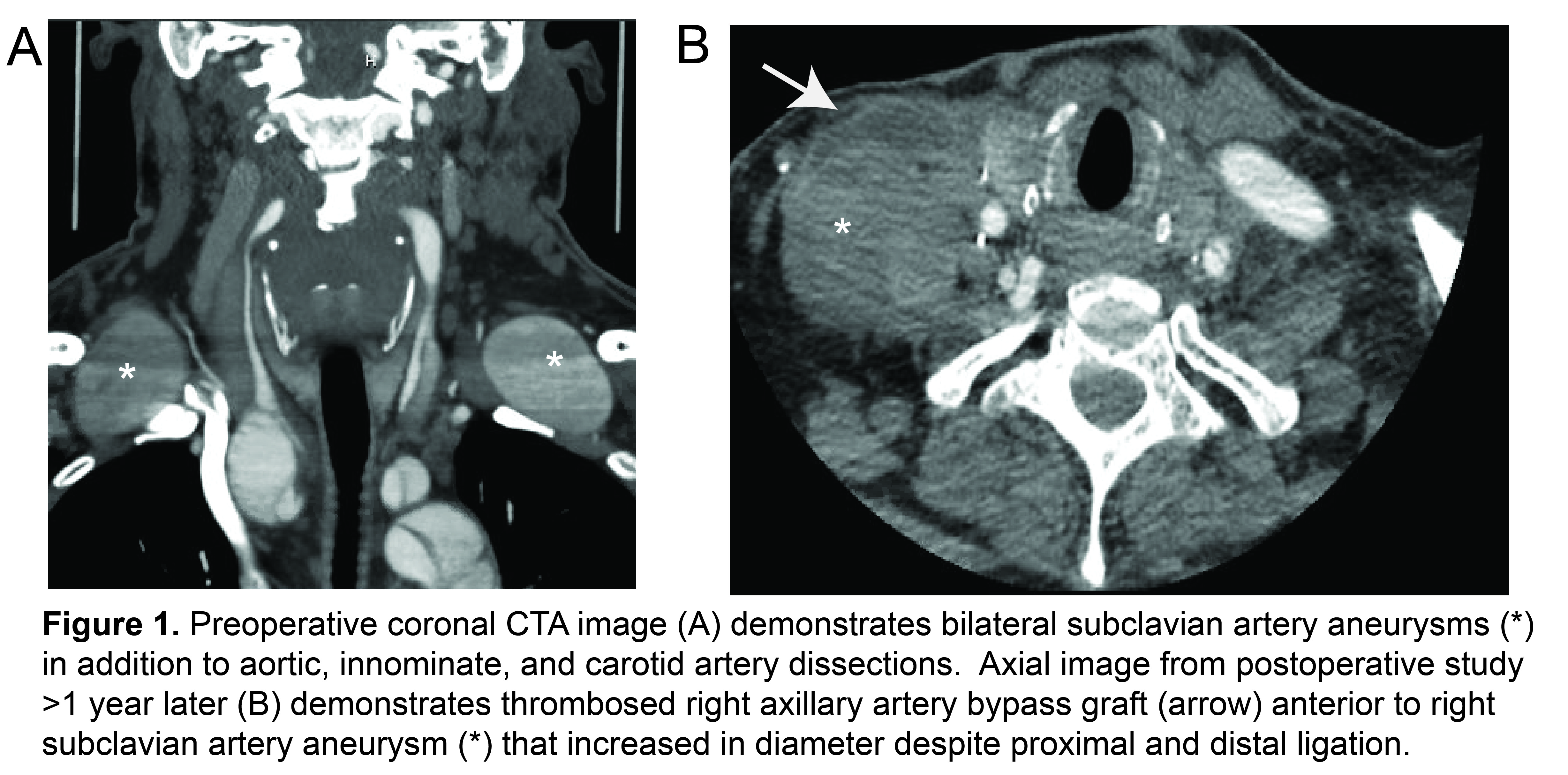
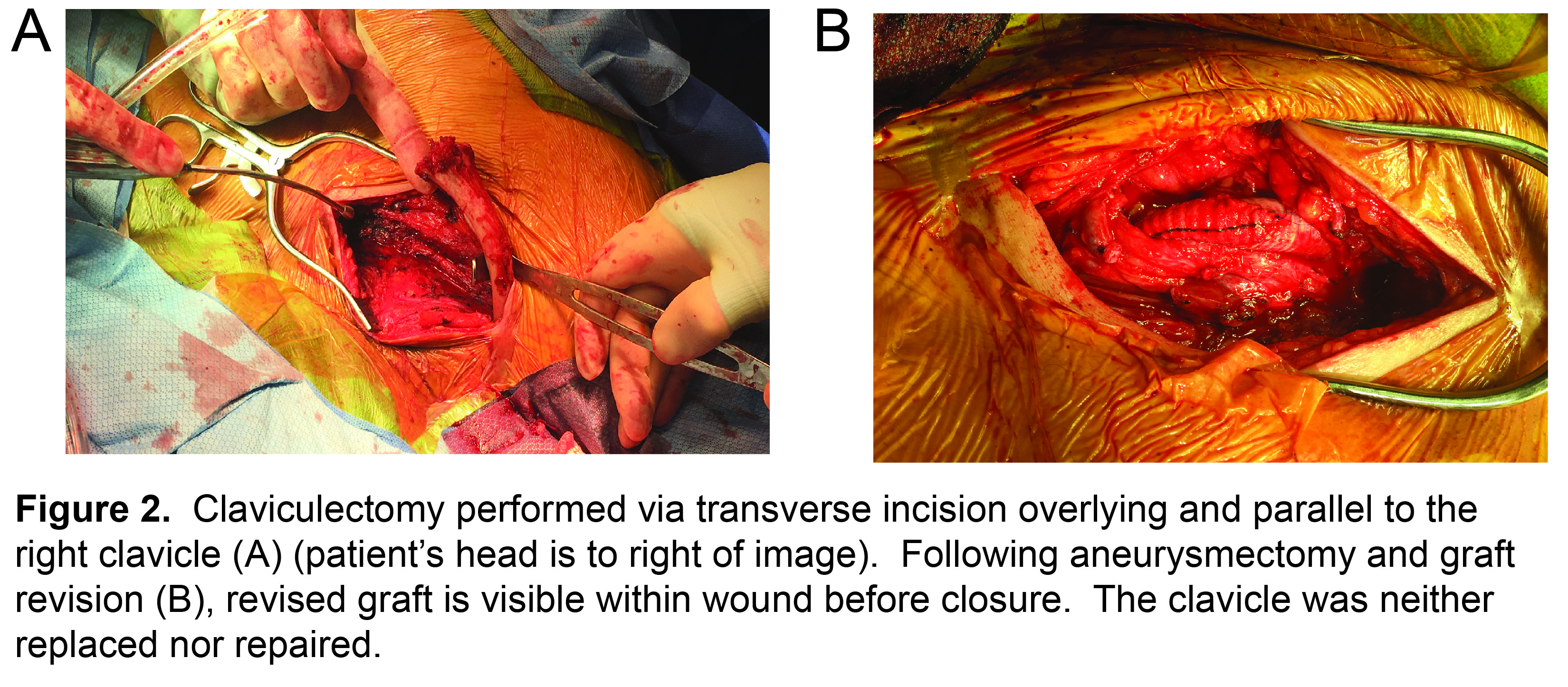
Introduction: Subclavian artery aneurysms (SAAs) are rare, and repair can be technically challenging for large aneurysms behind the clavicle. We report an unusual case of SAA expansion following initial proximal and distal ligation where claviculectomy, an uncommon but simple technique, greatly facilitated repair. Case Report: A 50-year-old man was referred to clinic following emergent aortic root replacement with mechanical aortic valve for repair of an acute Type A aortic dissection. The patient had bilateral pulsatile supraclavicular masses that were both palpable and visible. CTA demonstrated dissection involving the aortic arch and all arch vessels, a 43mm bi-lobed right SAA, and a 36mm left SAA (Figure 1A). Genetic testing revealed a heterozygous mutation of the FBN2 gene of uncertain significance. He was treated with redo sternotomy, deep hypothermic circulatory arrest, replacement of the ascending aorta and aortic arch, frozen elephant trunk, left common carotid artery bypass, bilateral axillary artery bypass, and transposition of the right carotid and bilateral vertebral arteries. Both subclavian arteries were ligated and divided, and the axillary grafts were tunneled beneath the clavicles with end-to-end distal anastomoses. Following repair, the patient had continued right SAA expansion to 57mm and thrombosis of the right axillary graft (Figure 1B). He also had effort fatigue and paresthesias of his right arm without signs or symptoms of limb-threatening ischemia. CTA suggested the right deep cervical and/or internal thoracic arteries as potential sources of ongoing SAA pressurization, but no endoleak was visible and neither of these vessels could be accessed during angiography. The patient was subsequently treated with claviculectomy, right subclavian aneurysmectomy with ligation of the right deep cervical and internal thoracic arteries from within the aneurysm sac, thrombectomy of occluded axillary artery bypass graft, and revision with a jump-graft to the distal right axillary artery. The resected clavicle (Figure 2) was neither replaced nor repaired. At one-month post-discharge, the patient reported resolution of his right arm effort fatigue, denied any functional limitations, and was cleared for resumption of normal physical activity and unrestricted physical therapy. Discussion: Claviculectomy is well-described for treatment of a variety of musculoskeletal conditions affecting the sternoclavicular joint. Reported outcomes indicate that most patients can expect full range of motion, acceptable cosmesis, relief of symptoms, and even regeneration of excised portions in younger patients. Claviculectomy is a simple procedure, although rarely performed by vascular surgeons for arterial pathology. In the current case, claviculectomy avoided a third sternotomy while facilitating direct surgical repair of a growing, previously excluded SAA while also allowing revision of a thrombosed vascular graft. Conclusion: Claviculectomy is a simple, well-tolerated procedure that greatly facilitates repair of large or complex SAA. Familiarity with this technique can expand options for surgical exposure and treatment of vascular pathology, including SAA.
Back to 2021 Abstracts