Massive Internal Carotid Artery Aneurysm Rupture Repaired Using Gore Hybrid Vascular Graft
Brandi M. Mize, Christine M. Dubberke, Lewis C. Lyons, III, Mohammed M. Moursi
University of Arkansas for Medical Sciences & Baptist Health-Little Rock, Little Rock, AR
Background: Aneurysms of the extracranial carotid artery (ECCA) are exceptionally rare, accounting for a minority of peripheral aneurysms. Incidentally found aneurysms should be closely monitored and surgical intervention highly considered to prevent debilitating complications like rupture, thromboembolic events, and cranial nerve palsies. Here we present a rare case of a massive ruptured right internal carotid artery (ICA) aneurysm extending to the skull base.
Methods: Chart review was performed for pertinent details relating to patient history, presentation, and operative management.
Results: A 74-year-old male with history of hypertension, hyperlipidemia, CAD, and known right ICA aneurysm (7cm in 2018) presented with acute enlargement and pain of his pulsatile right neck mass (Fig. 1). He never smoked, had no history of thromboembolic events, and took aspirin daily. He was hypertensive, but otherwise stable without focal neurological deficits (FND). CT angiogram revealed a contained, 9cm right ICA aneurysm rupture. He was taken emergently to the operating room. The right neck, upper chest, and right thigh (for potential vein harvest) were prepped. A longitudinal incision was made overlying the sternocleidomastoid’s anterior border. The proximal common carotid artery (CCA) and external carotid artery (ECA) were identified and controlled. The patient was systemically heparinized. After clamping the CCA and ECA, the aneurysm sac was entered, and hematoma evacuated. The ICA was found to be aneurysmal in its entirety, up to the skull base—making a standard anastomosis to the distal ICA not technically feasible. Given that neither revascularization nor traditional ligation was an option, a Gore Hybrid Vascular Graft (GHVG; W. L. Gore & Associates, Flagstaff, Ariz) stent was deployed into the intracranial portion of the right ICA to control backbleeding (Fig. 2). The stent was secured to the distal aneurysm sac to prevent retraction out of the skull base. The polytetrafluoroethylene (PTFE) portion of the GHVG was then oversewn and wrapped in aneurysm sac to prevent infection. Flow was re-established in the CCA and ECA. Recovery was uneventful without FND.
Conclusions: While the GHVG has been safely used for difficult revascularizations including ECCA aneurysm repair and rescue of unsuccessful carotid endarterectomies, this case demonstrates the novel use of the GHVG to oversew and ligate the distal ICA at the skull base in a setting where there was not adequate arterial wall to primarily oversew. GHVG utilization allows for expedited control of backbleeding and ligation without the need for disruption of the bony skull for more distal exposure.

Fig. 1 Patient with large, pulsatile, right neck mass.
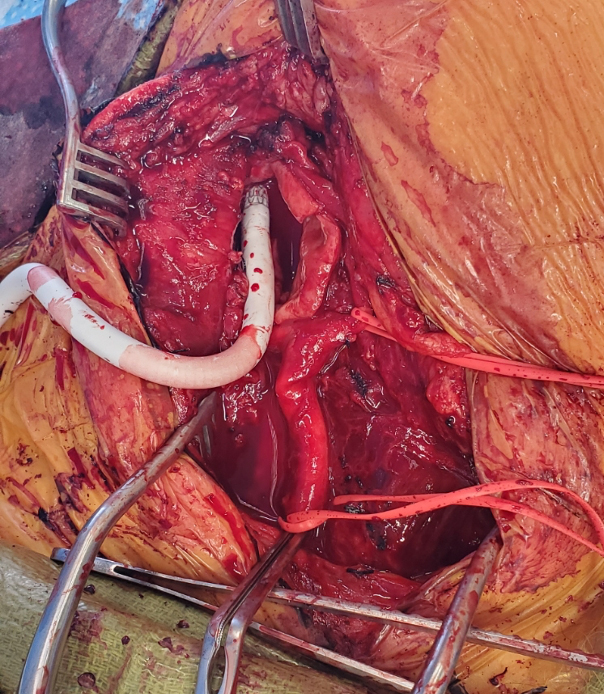
Fig. 2 GHVG shunt in distal right ICA orifice.
Back to 2021 Abstracts
