Contemporary Outcomes of Concomitant Supra-Inguinal Bypass and Infra-Inguinal Revascularization Procedures in Chronic Limb Threatening Ischemia Patients
Isaac N Naazie1, Isibor Arhuidese2, Omar Al-Nouri1, Nadin Elsayed1, Mahmoud Malas1
1University of California San Diego, La Jolla, CA; 2University of South Florida, Tampa, FL
INTRODUCTION: Combined supra-inguinal (SI) and infra-inguinal (II) revascularization procedures are sometimes necessary in patients with Chronic limb threatening ischemia (CLTI). However, data on outcomes of concomitant revascularization procedures are lacking. We studied the outcomes of SI bypass (SIB) in comparison to concomitant SIB with II bypass (IIB) or II peripheral endovascular intervention (IIPVI) among patients with CLTI
METHODS: A retrospective review of all patients with CLTI who underwent SIB (axillo-, aorto-, femoro-femoral) from January 2010 to June 2020 was conducted. Multivariable logistic and cox regression was employed to analyze outcomes. Outcomes were 30-day mortality, postoperative myocardial infarction (MI), postoperative major amputation, major amputation or death at 2 years and 5-year mortality
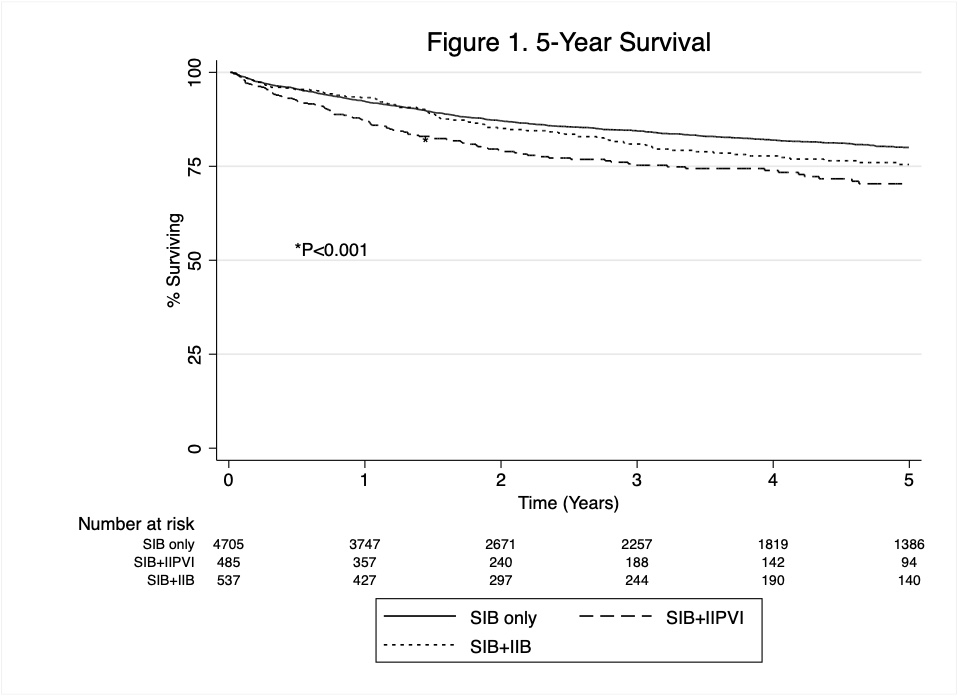
RESULTS: Of the 8,037 patients included, 81.3% (6,537) underwent SIB only, 8.9% (717) underwent SIB + IIPVI while 9.7% (783) underwent SIB + IIB. There were no significant differences in the adjusted odds of 30-day mortality, postoperative MI and perioperative major amputation between the three groups. However, when stratified by indication, there was a 2.8-fold increase in the odds of perioperative major amputation in both SIB + IIPVI (OR, 2.76; 95%CI, 1.30-5.88; P=0.008) and SIB + IIB (OR, 2.79; 95%CI, 1.38-5.54, P=0.004) among patients with rest pain but not those with tissue loss. Comparing SIB only vs SIB + IIB vs. SIB + IIPVI, 2-year amputation free survival was 83.4% vs 78.7% vs 75.3% (P<0.001), 5-year survival was 80.0% vs 75% vs 70.4% (P<0.001, Figure 1). There was no difference in 2-year major amputation or death and 5-year mortality between SIB only vs SIB + IIB. However, SIB + IIPVI was associated with 29% increased risk of major amputation or death in 2 years (HR, 1.29; 95%CI, 1.04-1.61; P=0.023) and 27% increase in 5-year mortality (HR, 1.27; 95%CI, 1.03-1.55; P=0.023), compared to SIB only. SIB + IIPVI was also associated with 41% (HR, 1.41; 95%CI,1.04-1.92, P=0.026) increase in 2-year major amputation or death and 43% (HR,1.43; 95%CI, 1.05-1.95; P=0.025) increase in 5-year mortality compared to SIB + IIB. This association persisted only among patients with tissue loss when stratified by indication (Table 1).
CONCLUSIONS: This study shows that patients with rest pain who undergo SIB with concomitant II revascularization have an increased risk of perioperative amputation. This could be due to increased complications risk of additional and often unnecessary II revascularization in patients with rest pain as opposed to tissue loss where additional revascularization is required. There is no difference in 2-year major amputation or death and 5-year mortality between SIB only and SIB + IIB. However, SIB + IIPVI is associated with an increase in 2-year major amputation or death and 5-year mortality relative to SIB only and SIB + IIB particularly in patients with tissue loss.
| Overall | Rest pain | Tissue loss | ||||
| Outcome | aHR (95%CI) | P value | aHR (95% CI) | P value | aHR (95%CI) | P value |
| 2-year major amputation | 0.91 (0.51-1.63) | 0.760 | 0.67 (0.26-1.74) | 0.407 | 1.15 (0.56-2.37) | 0.710 |
| 2-year major amputation or death | 1.41 (1.04-1.92) | 0.026 | 1.28 (0.76-2.14) | 0.352 | 1.52 (1.04-2.23) | 0.029 |
| 5-year mortality | 1.43 (1.05-1.95) | 0.025 | 1.38 (0.80-2.38) | 0.249 | 1.52 (1.04-2.24) | 0.032 |
Back to 2021 Abstracts