Vascular Event Occurrence in COVID-19 is Associated with Increased Mortality
Richard A Meena, Xiangqin Cui, Yue Xie, Milad Sharifpour, Luke P Brewster, Yazan Duwayri, Olamide Alabi
Emory University, Atlanta, GA
Background: The Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), the virus that causes Coronavirus Disease 2019 (COVID-19), emerged in December 2019 and quickly developed into a global pandemic that has had a profound impact on healthcare delivery, sociocultural norms, economic stability, and beyond. The disease severity can range from asymptomatic or a myriad of mild associated symptoms to severe acute respiratory distress with multi-organ failure and, potentially, death. There is emerging evidence suggesting increased rates of venous thromboembolism in patients with COVID-19. Additional nascent literature postulates that elevated D-dimer levels may be predictive of mortality. In response to such developments, multiple healthcare institutions have supported an expeditious approach towards prophylactic antithrombotic therapy with tiered anticoagulation escalation strategies in COVID-19 positive patients, albeit with little data to guide them. Thus, the overarching aims of this investigation include first, to estimate the incidence of thromboembolic events in a large academic health center network of multiple COVID-19 designated critical care units, and second, to explore the relationship between thromboembolic event occurrence and mortality. Methods: This study was approved by an academic health center network’s Institutional Review Board (IRB #00000601). All patients at least 18 years admitted for COVID-19 related illness between 3/15/2020 and 5/31/2020 to four hospitals within the aforementioned health center network were identified from a prospectively maintained database within the institution’s Corporate Data Warehouse. This administrative database houses demographic patient information that was utilized for analysis. Codes from the tenth revision of the International Classification of Diseases were used to identify patients with venous thromboembolism. The institution’s Corporate Data Warehouse was further queried to identify a comparison group of patients without COVID-19 who were admitted to intensive care units (ICUs) within the same network for acute respiratory distress syndrome (ARDS) or pneumonia between 1/1/2019 and 5/31/2020.
Given reports of additional vascular thrombotic events beyond venous thromboembolism in COVID-19 patients, such as arterial thromboembolism, coronary or cerebrovascular events deemed related to COVID-19 hypercoagulability, and recurrent extracorporeal circuit clotting during continuous renal replacement therapy (CRRT; defined as two or more clotting events), we analyzed a prospectively maintained dataset of consecutively admitted COVID-19 patients who required ICU admission and either developed or did not develop a vascular event. Specific data were obtained retrospectively from these patients by manual chart review to ensure the accuracy of diagnoses, as well as to obtain demographic data, identify high-risk comorbidities as identified by the Centers for Disease Control, review laboratory values associated with coagulopathy, and evaluate imaging or documented clinical suspicion of vascular events. Of note, routine venous thromboembolism screening or surveillance was not performed. Statistical analysis was completed using R programming, chi-square tests, t-tests, and multivariable logistic regression models.
Results: Overall, 4025 COVID-19 positive patients were admitted to four hospitals with designated COVID-19 ICUs within our health system. 187 (4.6%) of these COVID-19 admissions were diagnosed with venous thromboembolism. Venous thromboembolic events were seen more commonly in older (60.3 versus 50.2 years, p<0.001) and Black (65.2% versus 44.3%, p<0.001) patients. There were no statistically significant differences in birth sex when comparing patients with or without venous thromboembolic events.
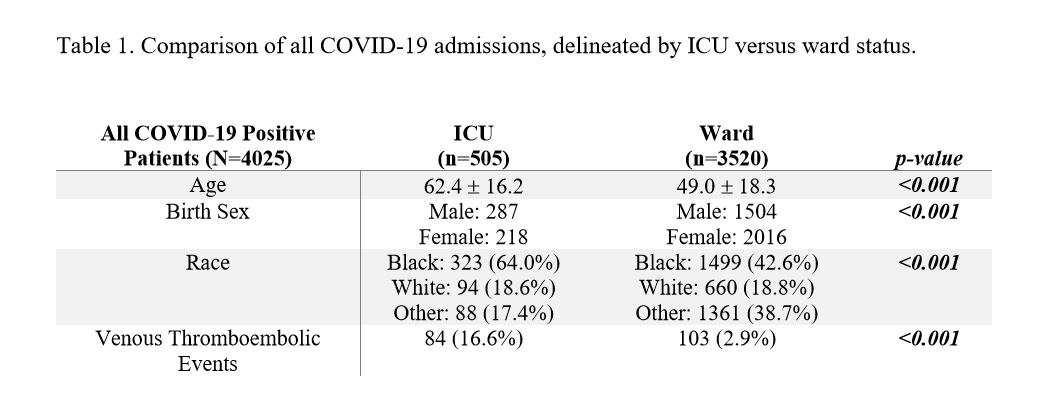
505 (12.5%) of the COVID-19 positive patients required ICU admission. Patients admitted to the ICU were notably older than patients who received care on the hospital ward (62.4 versus 49.0 years, p<0.001). As well, Black (64.0% ICU versus 42.6% ward, p<0.001) and male (56.8% ICU versus 42.7% ward, p<0.001) patients more often required ICU admission. The venous thromboembolic event rate in the ICU was 16.6%, compared to 2.9% on the ward (p<0.001, see Table 1). In comparison, 15.5% of non-COVID ICU patients with ARDS or pneumonia were found to have a venous thromboembolic event (p=0.35).
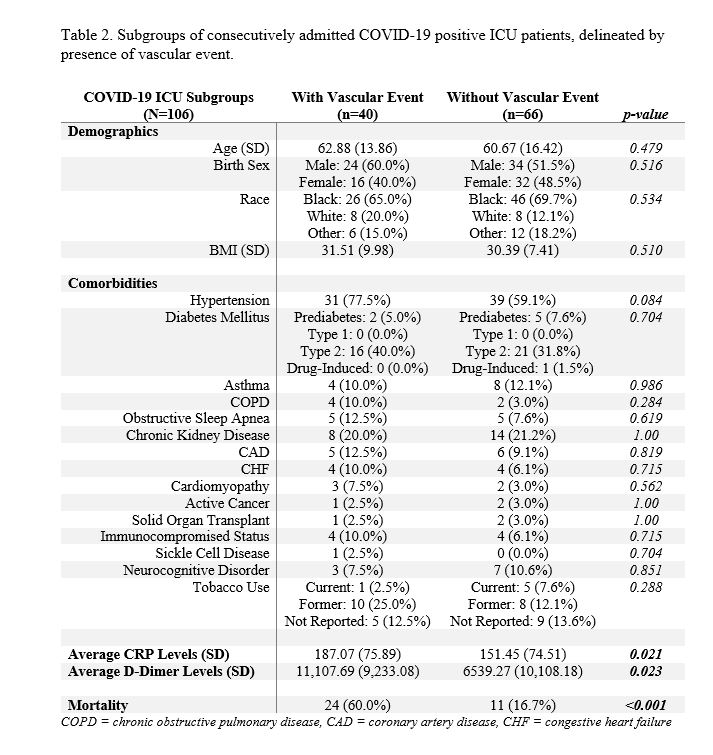
Forty COVID-19 positive ICU patients with 48 confirmed arterial and/or venous vascular events were further evaluated and compared to a control cohort of 66 COVID-19 ICU patients without vascular events. 37.5% of these vascular events were deep venous thromboses, 25% pulmonary embolisms, 16.7% acute coronary events presumed to be due to COVID-19 hypercoagulability, 14.6% CRRT clotting, 4.2% severe cerebrovascular accidents, and 2.1% upper extremity arterial ischemia. Elevated average CRP levels (187.07 versus 151.45, p=0.021) and average D-dimer levels (11107.69 versus 6539.27, p=0.023) were associated with increased odds of experiencing vascular events. Additionally, elevated maximum CRP levels (323.97 versus 261.13, p=0.007) and maximum D-dimer levels (35356.77 versus 15245.17, p<0.001) were associated with increased vascular event rates. There were no statistical differences in age, race, or birth sex between patients with or without vascular event, and there were no significant differences in predisposing comorbidities between the two cohorts (see Table 2). Twenty-four (60%) patients with confirmed vascular events died, compared to eleven patients in the control cohort (16.7%, p<0.001). Higher average CRP, average D-dimer, maximum CRP, and maximum D-dimer levels were all associated with increased mortality (all p<0.01), as was increased patient age (68.1 versus 58.2 years, p=0.002). On multivariate analysis of the matched cohorts (n=106), vascular events [odds ratio (OR) 15.6], age (OR >1.0), average CRP levels (OR >1.0), and average D-dimer levels (OR >1.0) were all independently associated with mortality.
Conclusions: In this large analysis, development of a vascular event was associated with 15-fold increased odds of mortality among critically ill patients with COVID-19. Further, older and Black patients hospitalized for COVID-19 were more likely to require ICU admission and to develop a vascular event. Average D-dimer and CRP levels did in fact correlate with higher rates of vascular events and were independently associated with mortality when controlling for age, race, and other potential confounders. Further elucidation of determinants that place a patient with COVID-19 at risk for a vascular event and a better understanding of anticoagulation strategies in this cohort may prove beneficial in terms of survivability and should be considered a high impact focus for future research.
Back to 2021 Abstracts