Outcomes of EVAR Conversion in Geriatric Patients Treated at A High-Volume Aorta Center
Christopher Jacobs, Salvatore Scali, Michol Cooper, Samir Shah, Dean Arnaoutakis, Martin Back, Scott Berceli, Gilbert Upchurch, Thomas Huber
Univeristy of Florida, Gainesville, FL
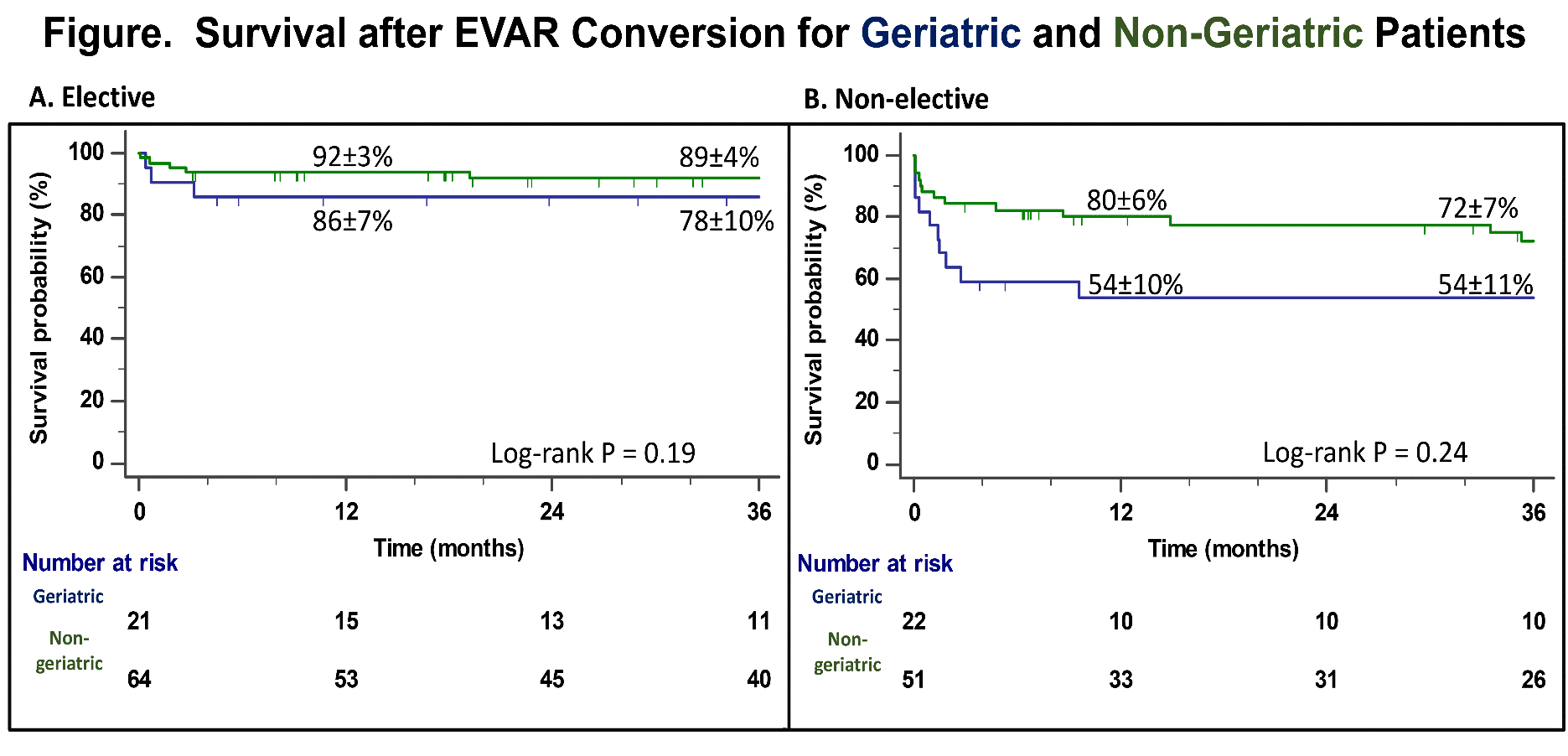
Introduction: Endovascular aortic aneurysm repair(EVAR) is the dominant treatment strategy for infrarenal AAA in geriatric patients. Correspondingly, EVAR failure resulting in subsequent open conversion(EVAR-c) has increased in older patients but there is a paucity of literature focusing on outcomes in this group. The purpose of this analysis was to evaluate our experience with EVAR-c in geriatric patients. Methods: Retrospective review of all non-mycotic EVAR-c procedures(2002-2019) at a single high-volume academic hospital with a dedicated aorta center(https://www.uf-health-aortic-disease-center) was performed. EVAR-c patients(n=158) were categorized into geriatric(≥80y;n=43) and non-geriatric(<80y;n=115) cohorts. The primary end-point was 30-day mortality. Secondary end-points included complications, readmission, 90-day mortality, re-intervention, and overall survival. Cox regression estimated effect of covariates on mortality risk. Kaplan-Meier methodology estimated survival. Results: No difference in pre-admission EVAR re-intervention rates was present(42% vs. 42%;p=1) although time to first re-intervention was greater in geriatric patients(41 vs. 15-months;p=.01). Concordantly, time to EVAR-c was longer(61 vs. 39-months;p<.01). No difference in rupture presentation with EVAR-c was evident(14% vs. 10%;p=.58); however, elective repair occurred less frequently(geriatric-42% vs. non-geriatric-59%;p=.07). AAA diameter was significantly larger for elective geriatric EVAR-c(7.8±1.9mm vs. 7.0±1.5mm;p=.02) and type 1a endoleak was the most common indication overall(58%;n=91). The overall 30-day mortality rate was higher for geriatric patients(age ≥80, 14% vs. age <80, 7%) but was not statistically significant(p=.21). Similarly, a trend towards higher 90-day mortality was identified for geriatric patients(23% vs. 10%;p=.07). However, incidence of any complication(56% vs 49%;p=.48), readmission(12% vs 6%;p=.32), unplanned re-intervention(10% vs 5%;p=0.5) and LOS(11 vs. 9 days;p=.34) was not different. Age ≥80 was not predictive of short-term survival; however, increasing comorbidity number, non-elective admission and renal/mesenteric revascularization increased 1-year mortality risk(Table). One and three year survival was not significantly different(Figure). Conclusion: Although a non-significant trend in higher peri-operative mortality occurred among geriatric patients, overall outcomes were comparable to younger EVAR-c subjects when treated at a high-volume aortic surgery center. This underscores the importance of appropriate patient selection and modulation of operative complexity when possible to achieve optimal results. Providers caring for geriatric patients with EVAR failure should consider timely elective referral to high-volume aorta centers to reduce resource utilization and frequency of non-elective presentation.
Back to 2021 Abstracts