Outcomes of Endovascular Aortic Repair in Connective Tissue Disease Patients
Suzanah Patterson1, Salvatore T. Scali1, Adam W. Beck2, Thomas M. Beaver1, Tomas D. Martin1, Dean J. Arnaoutakis1, George J. Arnaoutakis1, Gilbert R. Upchurch, Jr.1, Thomas S. Huber1, Martin S. Back1
1University of Florida- Gainesville, Gainesville, FL, 2University of Alabama-Birminghm, Birmingham, AL
INTRODUCTION: Open aortic repair(OAR) is the gold standard for connective tissue disease(CTD) patients, but results in mortality rates of 5-15% and 50-60% long-term survival even when treated at centers of excellence(COE). Durability concerns have led to clinical practice guidelines recommending against endovascular repair(ER) in CTD patients, but these lack Level I evidence and a significant knowledge gap exists. Therefore, the purpose of this study was evaluate outcomes of ER in CTD patients.
METHODS: A retrospective, single COE review was performed on consecutive ERs in CTD patients(2005-19). The primary end-point was aorta-related mortality. Secondary end-points were complications and freedom from secondary aorta-related intervention. Relative risk of selected variables with associated outcomes was determined and Kaplan Meier methods estimated freedom from end-points.
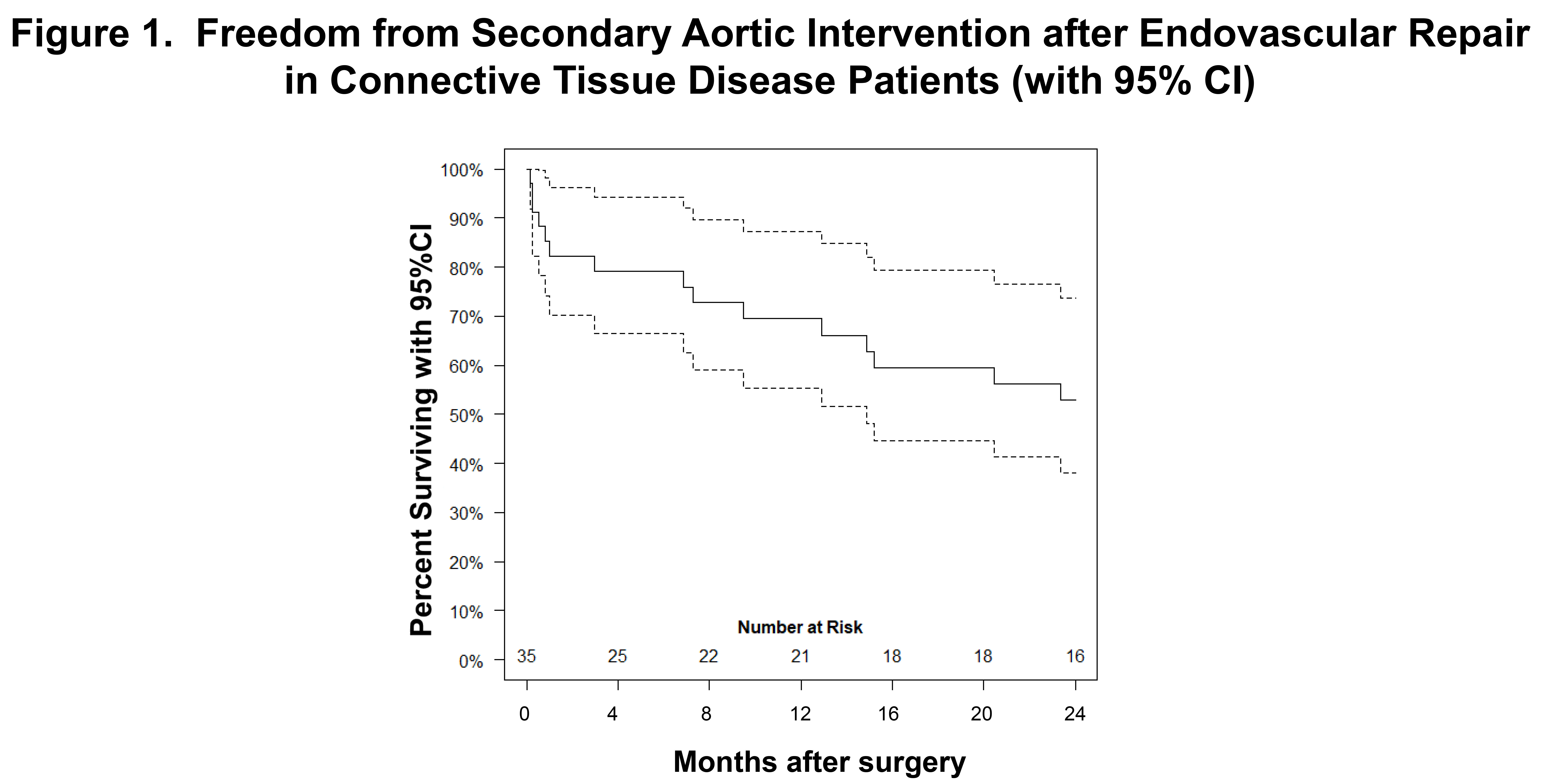
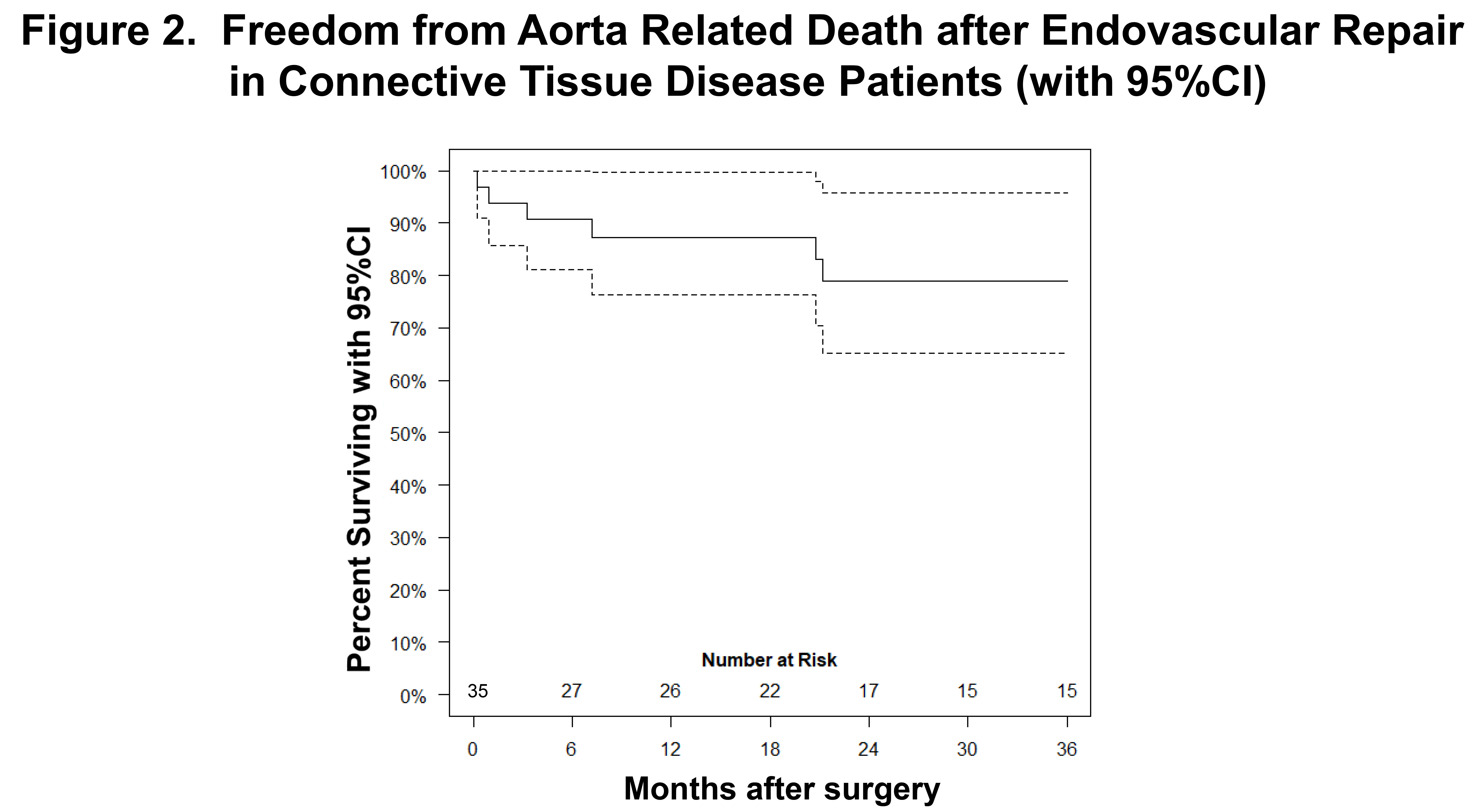
RESULTS: 35 patients underwent ER(median age 50, interquartile range[IQR] 34-61 years) and mean follow-up was 48±46(median 29[IQR 14-76]) months. CTDs included Marfan syndrome(86%;n=30) and Ehlers-Danlos(14%;n=5). A history of ascending and/or arch repair was present in 28(80%) patients. Patients were deemed unfit for definitive OAR due to surgical history(80%) and/or predicted poor outcome with OAR due to comorbidities(20%). Mean aortic diameter was 63±11mm and non-elective presentation occurred in 73%(n=25). Indications were predominantly for residual distal dissection after previous type A repair(acute complicated descending dissection-37%, thoracoabdominal false lumen[FL] aneurysm-46%) or post-surgical pseudoaneurysm(15%). ER types included: TEVAR(43%), simultaneous open repair with antegrade TEVAR(43%), fenestrated/branched ER(12%), and infrarenal EVAR(3%). The proximal landing zone involved Dacron in 60%(n=21). Median LOS was 9[IQR 5,22] days and 30-day mortality was 6%(n=2, both non-elective). Morbidity was 30%(n=10; retrograde dissection-1, reoperation for bleeding-2, respiratory failure-2, renal-1, unplanned 30-day SAI-6). In follow-up, any SAI occurred in 51%(n=18) and 17%(n=6) underwent >1 re-intervention. SAI indications included type 1/3 endoleak(28%;n=5), persistent FL perfusion/aneurysm(28%;n=5), type 2 endoleak(22%;n=4), juxta-aortic aneurysmal degeneration(17%;n=3), and remote aneurysm(6%;n=1). SAI events were non-elective in 56%(10 of 18) and one patient died within 30-days of SAI(6%). OAR involving (sub)total stent-graft explant occurred in 9(26%). One and 2-year freedom from SAI was 53±8%[95%CI 38-74%](Figure 1). Freedom from aorta-related death was 87±6% and 79±8% at one and 3-years, respectively(Figure 2). Risk of aorta-related death was not associated with acuity of presentation, age, indication, ER type, or occurrence of SAI. Previous arch replacement/proximal Dacron LZ did not associate with SAI or aorta-related mortality. Patients with ≥2 OARs before ER had increased risk of aorta-related death(OR 3.1, 95%CI 1.2-4.3;p=.03).
CONCLUSIONS: Results of ER appear comparable to historical OAR literature, with similar subsequent SAI and survival. Notably, ER may serve as a method to stabilize acute aortic syndromes and bridge to and/or reduce complexity of subsequent OAR. Life-long surveillance is required due to high SAI rates and history of multiple prior OARs appears to predict poor long-term outcomes.
Back to 2021 Abstracts